A Scottish woman feels virtually no pain due to a mutation in a previously unidentified gene, which could lead to breakthroughs in pain and anxiety treatments, a new research paper suggests.
Researchers from the University College London and Oxford University also discovered that, due to a genetic mutation, a 66-year-old woman’s wounds healed significantly faster than normal. The mutation also led to her feeling very little anxiety and fear throughout her life.
The study’s lead researcher Dr. James Cox said understanding the mutation could help guide the development of new treatments for a wide variety of conditions.
"We found this woman has a particular genotype that reduces activity of a gene already considered to be a possible target for pain and anxiety treatments," Cox said in a press release.
The study, which was published in British Journal of Anaesthesia on Wednesday, explained how the 66-year-old woman hadn’t needed painkillers after surgeries throughout her life, had injuries that healed very quickly and had a lifelong history of cuts and burns she never felt.
She told researchers she hadn’t noticed some burns until she could smell her flesh burning.
HER MUTATION CAME TO LIGHT AFTER HER HIP SURGERY
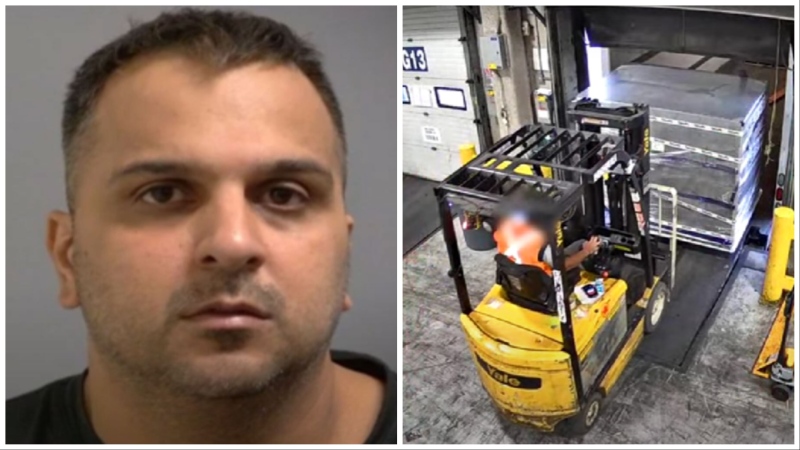
She first came to researchers’ attention when she was 65 years old and she had sought treatment for her hip, which had suffered severe joint degeneration.
She told BBC News she only knew something was wrong not because of any pain she felt, but because the degeneration had it made it physically difficult for her to walk.
But unlike most sufferers, she felt virtually no pain. She similarly felt no discomfort a year later, after she underwent surgery on her hand -- which was unusual because recovery is normally extremely painful.
In a phone interview with CTVNews.ca, Cox said, "to feel pain is really important for protection. So to not have that warning system is potentially problematic."
Pain geneticists later found she had two notable mutations.
One mutation was inside a pseudogene -- an imperfect copy of a functional gene -- and the second mutation was in the neighbouring FAAH gene that controls an enzyme central to pain sensation, mood and memory.
Researchers had assumed the pseudogene was a “junk” non-functioning gene but have now realized it likely controls how the FAAH gene works.
Mice without the FAAH gene didn’t feel as much pain, had accelerated wound healing and reduced anxiety. The Scottish woman had similar traits.
She earned the lowest score on a common anxiety scale and describes herself as an optimist. She recalls how she rarely panics -- even in dangerous situations such as a recent traffic incident she was involved in.
She also reports memory lapses throughout her life such as forgetting words or keys, which has previously been associated with mutations in the FAAH gene.
"We hope that with time, our findings might contribute to clinical research for post-operative pain and anxiety, and potentially chronic pain, PTSD and wound healing, perhaps involving gene therapy techniques," said Cox.
The co-lead author of the paper, Dr. Devjit Srivastava, said the “implications for these findings are immense.”
As for the Scottish woman, who was unnamed in the paper, she said “I would be elated if any research into my own genetics could help other people who are suffering."