Ontario has become the first province to list an inexpensive and well-known antidepressant as a treatment doctors can “consider” for patients with a mild COVID-19 infection in a bid to keep them out of hospital.
In the science table listing on Wednesday, a panel indicated that the drug fluvoxamine can be considered and prescribed to patients with a mild case who are at risk of having more severe symptoms.
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) antidepressant that is typically used to treat depression and obsessive-compulsive disorders.
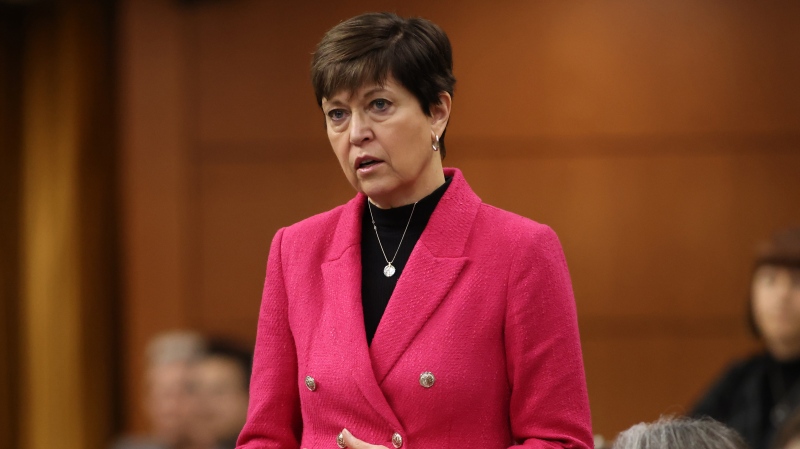
“Right now, we're in a really unprecedented wave of Omicron and we have just a staggering number of patients getting infected,” Dr. Menaka Pai, associate professor of medicine at McMaster University and co-chair of the Ontario COVID-19 Science Advisory Table, told CTV News. “Our goal is to keep them safe, to keep them out of hospital and also to preserve our scarcest resource, which I would say is our hospital beds.”
The drug costs a little more than a dollar a day and would be taken for 15 days, starting with a small dose. In comparison, the antivirals medicines from Pfizer and Merck cost nearly $1,000 dollars per patient.
Studies have shown that the drug can cut hospital admissions due to COVID-19 by up to 30 per cent.
“When you look at all that data together, it is very likely that fluvoxamine prevents hospitalization in patients with mild COVID-19,” Pai said. “So patients who are not yet on oxygen, and if our goal in this wave of the pandemic is to stop patients with COVID from ending up in those scarce hospital beds, then that I think is a very important finding, indeed.”
Researchers at McMaster University monitored more than 1,500 unvaccinated COVID-19-positive patients for a month and gave them either the drug or a placebo.
Of those who received fluvoxamine, 10.6 per cent required treatment by a doctor for more than six hours or were hospitalized, while 15.7 per cent of the participants who received a placebo were hospitalized or needed physician treatment for more than six hours. When patients took all of their drugs, the noted beneficial effect went up to 65 per cent, the study found.
Dr. Edward Mills, the co-principal investigator of the trial, said the results could be a game-changer, particularly in developing countries with low vaccination rates.
“It’s a very large treatment effect, one that hasn’t been observed for any drug yet,” he told CTV News back in October when the study was published.
John’s Hopkins University has also endorsed the drug for use within seven days of symptoms, provided the patient is not in their third trimester of pregnancy.
While Ontario is the first province to list the drug as an option, Pai said other regions are also considering the medication as a possible preventative therapy.