TORONTO -- A new Canadian-led study is pulling back the curtain to reveal the genetic triggers for the most common form of brain cancer in children.
The researchers responsible for the work say that by identifying what is going wrong in brain cells when these tumours begin to grow, better -- and less toxic -- treatments can be developed.
Some of the findings even hold out the hope that existing drugs may be useful in some cases, said Dr. Michael Taylor, a pediatric neurosurgeon and molecular geneticist at Toronto's Hospital for Sick Children.
"Instead of spending 15 years and a billion dollars to develop a new drug, we hope to be able to short-circuit that process, use drugs that are already available, already tested and thereby improve the outcome for our children," Taylor said in an interview.
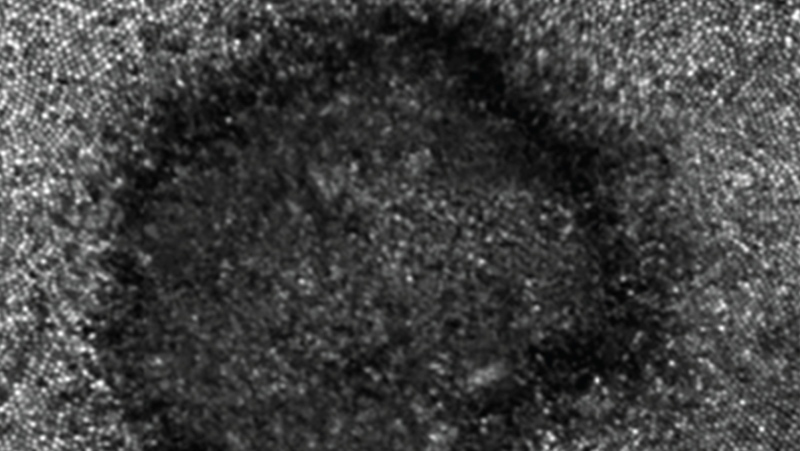
The cancer is called medulloblastoma. Every year in Canada between 30 and 40 infants are diagnosed with this type of cancer.
About 70 per cent of children who receive the diagnosis survive, but the cure comes at a very high cost.
The treatment involves surgery, chemotherapy and radiation. In fact, the entire brain and spinal column are treated with radiation multiple times. That leads to a permanent drop in IQ -- on average between 10 and 20 points. The children often face radiation-related health problems later in life, including infertility and a higher risk of developing other cancers.
There are four types of medulloblastomas, each with a different survival rate and genetic features. WNT, the least common form, has a nearly 100 per cent cure rate. Group 3 tumours, on the other hand, are almost invariably fatal. The other two types are called Sonic Hedgehog and Group 4.
Despite the different prognoses, the cancers are all treated the same. But this ongoing project, called the Medulloblastoma Advanced Genomics International Consortium, or MAGIC, is raising hopes that may not be necessary.
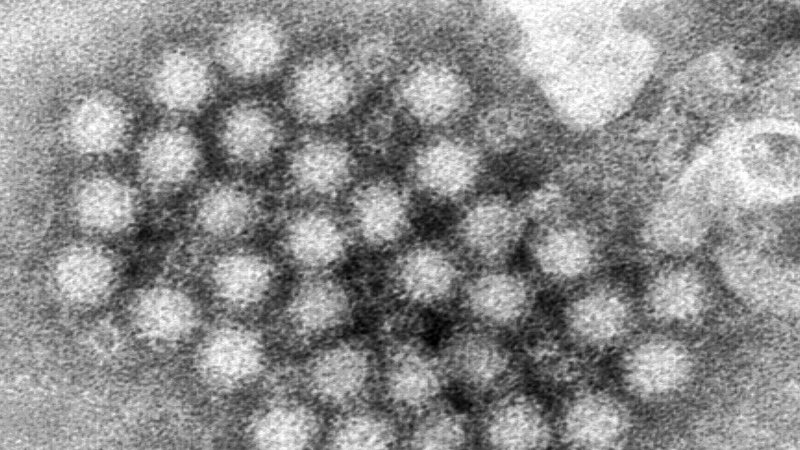
In the work, scientists from Sick Kids and BC Cancer Agency's Michael Smith Genome Sciences Centre used advanced genetic tools to look for the molecular changes in the cancer cells that trigger the different types of medulloblastoma.
Their findings were published Wednesday in the journal Nature.
The work is the product of an enormous international collaboration, with doctors from around the world supplying tumours to be studied. Looking at large numbers of tumours -- 1,087 in total -- allows the scientists to start to see the patterns that would not be visible if they looked at only a small number of tumours.
"From this type of study we have a clear message, which is: Guys, if you want to do better, you have to clearly see deeper in the tumour and figure out what are the reasons why you fail in some patients," said Dr. Eric Bouffet, a pediatric neuro-oncologist at the Hospital for Sick Children who is also an author on the paper.
Already there are intriguing clues. For instance, mutations spotted in Group 3 medulloblastomas are also known to occur in some adult cancers and some non-cancer adult diseases. And a number of pharmaceutical companies are working on drugs for those adult diseases that may work in children as well, Taylor said.
In the nearer term, the findings may reap benefits for children diagnosed with medulloblastomas of the WNT subtype.
Given the high cure rate for this form of the disease, doctors are interested in seeing if a less toxic approach could be used on these children -- maybe even skipping radiation. Bouffet said trials to test the hypothesis are being designed.
The ongoing research is being funded by a number of agencies, including Genome BC, Genome Canada and the Terry Fox Research Institute.