Tim Boyce was in desperate need of help.
The Canadian soldier had been in a downward spiral for several years. In 2006, he had been diagnosed with post-traumatic stress disorder, anxiety, severe depression, anger issues and several addictions. He says he began isolating himself and started drinking, doing drugs and gambling. His wife left him, taking his young daughter with her.
Last year, he was contemplating suicide. He says he had counted on the military for help. What he was given was the number of a help line.
“I called that number 17 times, the second time I let it ring 23 times and I gave up,” he told CTV News. “There isn't the ability. What good is it going to do me?”
Boyce joined the Armed Forces in 1990. He served in war zones overseas, and says he witnessed mass graves, bombings and death on a daily basis, all of which he says has contributed to his fragile mental health.
He says his condition is so bad now that he lives in a house with blacked-out windows. He says he has no friends or is able to maintain any relationship with his family. He shops at 3 in the morning to avoid crowds.
And he says he’s still advised by the military to call that same hotline when he reaches low points.
“Another time I was sent to an answering machine. Not very good to send a person on the verge of suicide to an answering machine,” he said.
Sadly, Boyce’s story isn’t unique. While in recent years there has been an effort to increase awareness about where people can turn to when they’re suicidal, some Canadians are not getting the help they need. Last Sunday, CTV`s medical specialist Avis Favaro told the stories of three Canadians who sought the help of professionals but whose cries were not taken seriously.
While it’s hard to know if immediate help in each of these cases would have saved lives, serious questions are being raised about what changes need to be made to get assistance to people who need it the most. And some believe Quebec’s system of immediate response could serve as the model for the rest of the country.
Not isolated events
Favaro’s report on the issue has generated a huge online response, with Canadians from across the country writing in with their own stories about how their loved ones fell through the cracks when they sought help.
One commenter named DP wrote that she and her husband took their son to the hospital in 2010 because he had tried to commit suicide. She wrote that the hospital sent him back home, saying that “he wasn't bad enough.” Her 26-year-old son later killed himself, she said.
Another commenter, JH, wrote that: “Three years ago my dad was taken to emergency on three separate occasions because he was suicidal. The psychologist told my dad to take his medication and sent him home. She refused to admit him, even though it would have saved his life. Two months later he hanged himself in the garage where my mother found him a few hours later.”
Dr. Stan Kutcher, an internationally-renowned expert in the area of adolescent mental health, says these types of failures are simply unacceptable.
“I find it incredibly frustrating that the movement in the health care system -- although it's better than it used to be -- still isn't where it should be,” he said. “Probably the most effective intervention is rapid access to health professionals who can rapidly diagnose and treat mental disorders and provide social community support during a time of crisis. We know that. The problem that we have is that the data has not necessarily been translated into policy or practice.”
A better model?
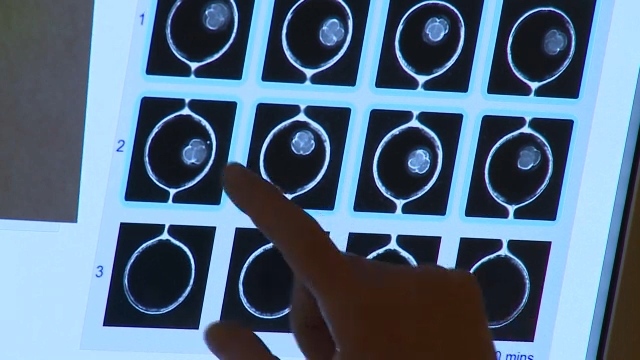
Quebec once had the highest suicide rates in the country until some regions of the province instituted the Close Follow Up Program, essentially a system of rapid hospital response for suicidal patients.
As soon as patients reach out to a hospital because they are suicidal, they are targeted for quick assessment and treatment, and also linked with a counsellor for ongoing visits starting within 24 to 48 hours.
“So as soon as someone is reaching to the hospitals or reaching to a service, we need to give to provide to those persons good services because their life is on the line,” Bruno Marchand said, the director of Quebec’s suicide prevention association.
The preliminary results are so encouraging that organizers say they are hoping the program expands across the whole province. They also think it could be a template for hospital and suicide hotline services across the country.
“If we don't act and act quickly we might have problems,” said Marchand. “We might lose lives that we could have saved.”
With a report from CTV medical specialist Avis Favaro and producer Elizabeth St. Philip
If you or someone you know needs to connect to a suicide hotline, please call a local distress or crisis centre listed here or 1-800-SUICIDE (1-800-784-2433)
If you have a family member who experienced similar problems while suicidal, please follow this link to write to us.