A University of British Columbia professor and emergency room doctor is calling for ketamine to be available for paramedics as an option for their patients’ pain relief after he was left with few choices following a near-death experience.
Dr. Gary Andolfatto, an assistant clinical professor at the school’s department of emergency medicine, suffered a broken femur following a bicycle crash in December 2014 and was forced to drag himself using his bike as a crutch for four hours while he searched for help.
Once Andolfatto finally found someone capable of calling 911, paramedics arrived on the scene but they could only offer nitrous oxide, known as “laughing gas,” to help alleviate his agony during a 45-minute ambulance ride to the hospital.
“I get in the back of the ambulance and I asked the paramedics: ‘OK, what have you got for me for pain? Because I could really use something,’ and I was quite shocked to discover that the answer was essentially nothing,” he told CTVNews.ca in a phone interview. “That whole 45-minute trip, I listened to this impassioned plea from the paramedic in the back with me about how this situation happens to them all the time.”
This experience led Andolfatto to his latest research -- recently published in the journal Annals of Emergency Medicine-- in which he found that a ketamine nasal spray combined with nitrous oxide can provide clinically significant pain relief for patients within 15 minutes of receiving the treatment compared to the nitrous oxide alone.
In British Columbia, advanced and critical care paramedics are allowed to administer ketamine as a pain-relieving option, but 70 per cent of paramedics in the province do not have this qualification and thus are only allowed to give nitrous oxide to their patients.
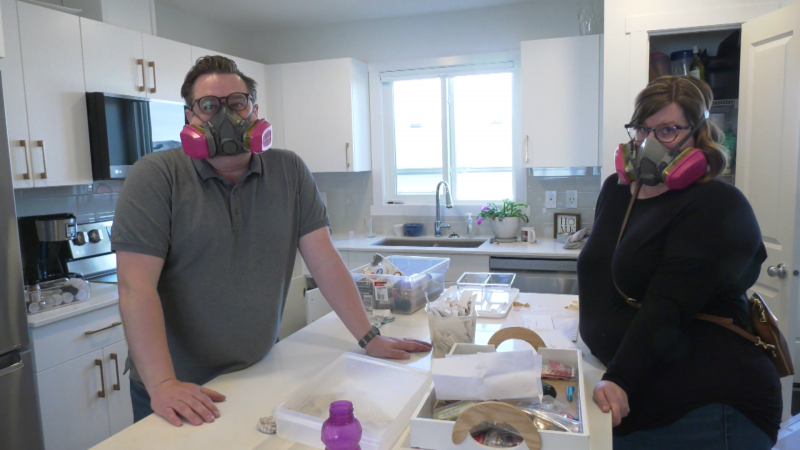
As part of Andolfatto’s study between November 2017 and May 2018, paramedics across the province gave 120 patients suffering from acute pain nitrous oxide for relief, while half of those patients were also given ketamine in the form of a nasal spray. The other half were given a saline solution spray as a placebo.
“What we found was that the patients who received ketamine were much more comfortable and had much better pain control than those that received the placebo,” Andolfatto said.
According to the Centre for Addiction and Mental Health, ketamine is typically used as an anesthetic and painkiller among veterinarians, though it is also sometimes used in human medicine. It is also known as a recreational drug under the street name “Special K.”
Andolfatto said ketamine is the ideal drug to help paramedics treat patients in pain because it’s cheap, effective, easy to use and can be given to someone sitting up or lying down. He adds a morphine treatment can impact a patient’s breathing if not administered properly, but that sideeffect is not present with ketamine usage.
“Essentially, it’s impossible to kill someone, even if you mess up totally,” he said.
Andolfatto hopes this research will open the doors to the possibility of ketamine being available to paramedics across the globe.
“I actually consider this a worldwide problem and B.C. is certainly no exception to that,” he said. “There’s loads of literature out there, people publishing studies about the difficulties and the challenges with providing early pain control to people, especially in the pre-hospital setting.”
For now, Andolfatto is in the process of implementing ketamine nasal sprays in ambulances across British Columbia, one community at a time.
“It’s being done slowly and carefully, which I think is the sensible way to do this, because (there are) all sorts of logistics that need to fall into place,” he said.