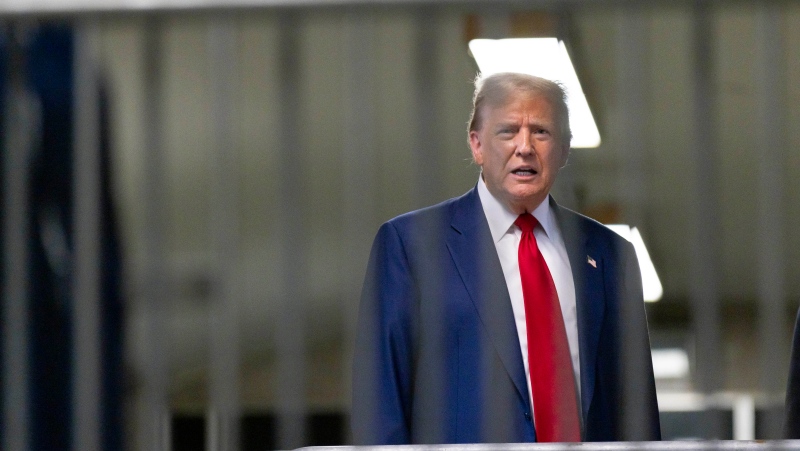
As Toronto Mayor Rob Ford begins chemotherapy for the liposarcoma tumour in his abdomen, doctors may need to try several drugs before they find one that works. But there's hope of better treatments to come in the future through a new technology called "precision medicine."
Cancers are notoriously varied, so even two patients with the very same kind of cancer will respond differently to the same chemotherapy medications. That's because as tumours grow, the genes in the cancer cells mutate in different ways. For every type of cancer, there are different mutations.
Quickly finding the right drugs that will work on these growing tumours is critical, since the side effects of chemotherapy can be devastating.
Now, doctors have found a new way to learn more about the genetics on a patient's tumour, to guide them in their search for the right drug.
A research firm in the U.S. called Champions Oncology developed something it calls Tumorgraft. It takes a small sample of the patient's tumour, and implant them into specialized mice that have been bred without immune systems. The lab then tests different drugs to see which works best on the mice. Since the mice have no immune systems of their own, the researchers can be sure it's the drugs that cause tumours to shrink in some of the mice.
Toronto resident Yaron Panov has undergone precision medicine for the same kind of cancer Ford has: pleomorphic liposarcoma. When Panov was diagnosed in 2010, doctors tried surgery, but the treatment failed and after just three months, the tumour grew back and spread.
Doctors suggested chemotherapy but were not optimistic for Panov's chances.
"I was given just a few months to live," he told CTV News.
Panov's wife, Dr. Rochelle Schwartz, herself a physician, had heard about precision medicine treatments being developed at Champions Oncology and the couple flew to the States.
There, testing on lab mice implanted with Panov's tumour cells revealed that the usual chemotherapy drug that would have been given to Panov would not have worked on him. But a drug developed for colon cancer, on the other hand, showed excellent effectiveness.
Panov underwent chemotherapy with the drug. While the treatment was difficult, causing him fatigue, intense nausea and hair loss, it worked to shrink his tumour.
Panov still has more chemotherapy in the future to maintain the tumour shrinkage, but for now he is feeling optimistic.
"He had a CT scan 6 weeks ago, and he is tumour-free -- to the astonishment of the sarcoma team," says his wife, Rochelle. "It helped to save his life."
The new treatment didn't come cheap. The lab work on the mice was expensive, and so was testing each drug. The entire testing procedure can be time-consuming, taking sometimes several months during which a patient may become sicker.
Dr. Peter Metrakos, the program leader at McGill University Health Centre's Cancer Research Program, says several researchers in both the U.S. and Canada are doing similar work, using patient-derived cells and grafting them into mice. But he says the branch of research is still very new.
"There have been dramatic responses by tailoring the therapy with this approach. But I don't think it is prime time yet. I think there is still a lot of work to be done," he told CTV News.
Nevertheless, Panov and his wife want to bring the approach to Canada so that Canadians with all kinds of cancer can benefit. They have started the Panov Program in Precision Chemotherapy, a project with Mount Sinai Hospital in Toronto and Champions Oncology. The goal is to raise $1.5 million for a study to validate the Champions approach.
Schwartz believes targeted therapies would save many cancer patients from trying difficult treatment drugs that are bound to fail. What's more, targeted treatment would likely be cheaper than giving patients expensive medications to patients that won't work.
"Isn't it better to give the patient the right chemo the first or second time so they don't suffer from horrible side effects?" she says.
With a report from CTV's medical specialist Avis Favaro and producer Elizabeth St. Philip