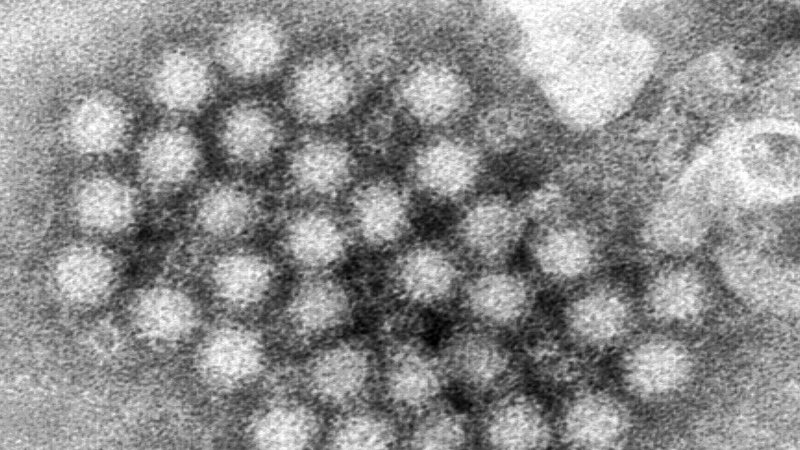
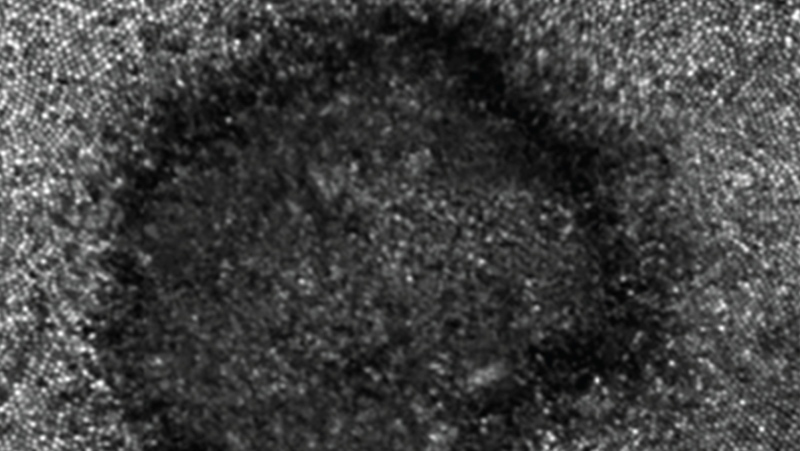
The Zika virus is spread almost exclusively by mosquito bites, and has been native to parts of Africa and Asia for decades. It was recently introduced into the Americas, namely Brazil, where it is believed to be linked to a surge in miscarriages and birth defects.
The geographic reach of the virus encompasses 22 subtropical and tropical countries, and the World Health Organization anticipates that the entire Western Hemisphere (except for Canada and Chile) will see locally acquired cases within the next year.
The spread of the virus in the Americas has prompted the WHO to declare Zika an international emergency.
Why has Zika been declared an international emergency?
After convening an emergency meeting of independent experts, the World Health Organization said the explosive spread of the virus in the Americas is an “extraordinary event” and a “public health threat to other parts of the world.”
Such emergency declarations can trigger increased funding and efforts to stop an outbreak, as well as prompt research into possible treatments.
How does the Zika virus spread?
Zika belongs to the same family of viruses as dengue fever and West Nile, and is spread among humans via mosquito bites in the same way as malaria, dengue fever and Chikungunya.
International spread of the virus occurs when someone who is already infected with Zika arrives at a new location, and is bitten by a mosquito that then transmits the virus onto another person. A concern with Zika is that the species of mosquito so far responsible for its spread, Aedes aegyptii, is common throughout the Western Hemisphere and could therefore quickly propagate the virus.
Who is most at risk?
Expectant mothers are the only people who need to worry about travel to affected countries. A woman residing in Hawaii who spent one month in Brazil early in her pregnancy gave birth to an infant with microcephaly (a birth defect featuring an unusually small head) and brain damage. Preliminary tests (full details not yet available from the CDC) indicate that this is linked to Zika virus.
WHO officials said the only known cases of microcephaly associated with Zika are from Brazil.
Does the virus travel from human to human?
Generally not, but potentially through a blood transfusion, or perhaps through a health care worker injury from blood taken from an affected patient with Zika.
Can Zika be transmitted through sexual contact?
In some circumstances, yes. In early February, the U.S. Centers for Disease Control confirmed a Zika virus case in Texas that was acquired through sexual transmission.
Dallas County said that a patient was infected with the virus after having sexual contact with an ill individual who returned from a country where Zika virus is present.
This is not the first time the Zika virus has been linked to sexual transmission. A 2011 study looked at two cases of the virus in U.S. scientists who lived in Senegal. When one of the scientists returned home and fell ill, his wife also contracted the virus. She had never been to Africa or Asia.
According to authors of the 2011 study, circumstantial evidence suggested direct person-to-person spread, possibly through sexual contact.
It is not clear whether sexual transfer of Zika is reciprocal, or if it can be passed along through only males or females.
The outstanding question is whether sexual transmission of the Zika virus is a rare occurrence, something the CDC and WHO will likely examine. In light of the case showed male-to-female transmission, the CDC has revised its advice for pregnant women whose sexual partners have travelled to or live in areas with active Zika virus.
"You should abstain from sex or use condoms the right way every time you have vaginal, anal, and oral sex for the duration of the pregnancy," the CDC says.
Is the link between the virus and birth defects confirmed?
The jury is till out on this issue. Evidence is mounting in favour of Zika as the cause of some of the unusually high number of microcephaly cases in Brazil between October 2015 and January 2016: approximately 3,500. According to a preliminary analysis carried out by Brazilian health authorities, the risk of microcephaly appears to be greatest with infections acquired during the first trimester of pregnancy. Nevertheless, the WHO warns that evidence linking the virus and the spike in microcephaly remains circumstantial.
Officials say they plan to investigate any links between the virus and the birth defects by looking into other possible factors, such as co-existing infections, environmental influences and toxins.
Is there a vaccine?
There is no vaccine that protects against Zika virus infection, nor is there any antiviral medication to treat it.
Can a person be tested for Zika?
Though Zika testing is being performed at the CDC, and soon at the National Microbiology Laboratory, a rapid, reliable easy to perform test is still under development. Therefore, if, say, a pregnant patient were tested now, a long delay in obtaining results would be expected.
Which countries are most concerned with active human cases of the Zika virus?
Brazil is not the most common "sun destination" for Canadian holidayers. The virus has reached Central America and the Caribbean, with cases reported in Nicaragua, Panama, Mexico, St. Martin, Martinique and Guadeloupe.
Southern parts of the U.S. may soon be affected too, according to the WHO. Here is a link to the most recent CDC list of countries identifying locally acquired cases.
Has the virus travelled to other countries?
Numerous tropical destinations now have ongoing local transmission of Zika, though only Brazil has reported cases of microcephaly thus far. Brazil has the largest population of the countries affected thus far; it likely takes many Zika infections (even in pregnant women) to start seeing cases of microcephaly. It is important to keep in mind that all cases being identified in Canada and the U.S. have been acquired during travel abroad.
Might Zika arrive in Canada, like West Nile did?
Canada’s public health officer says the threat to Canada from the Zika virus is “very, very low.” The northern parts of North America (Canada and the Northern U.S.) are unlikely to have sustained spread of Zika, mainly because the wrong mosquito species predominates.
How would Zika make it here?
First, someone with active Zika virus infections has to fly home and be bitten by a mosquito. Keep in mind that most Canadians go down South during our winter; when they return there are no mosquitoes around to spread the virus from a returning traveller. But for argument's sake, suppose someone brought home a Zika infection during the summer. As we don't have the Aedes aegyptii mosquito species here in Canada, a different Aedes mosquito species – limited to Southern Ontario – might be the only one to carry Zika. This mosquito would then have to survive a winter with the virus to spread the disease over the next season.
By contrast, West Nile virus affects a different prevalent mosquito species (Culex species), and is here to stay year after year because it "overwinters" easily. This is why we see West Nile virus cases year after year.
Should I hold off on giving blood in Canada?
In early February, Canadian Blood Services confirmed that anyone who has travelled to places apart from Canada, continental U.S. and Europe will now be temporarily ineligible to give blood for a period of 21 days upon return to Canada. CBS said the three-week period “ensures enough time has passed for the virus to be eliminated from a person’s bloodstream.” The three-week period of blood-donation ineligibility begins the day the traveller returns to Canada.
What are the symptoms to watch for?
Symptoms are similar to Dengue Fever: fever, rash, joint pain and light sensitivity lasting a few days, starting within 10 days of coming from a Zika-affected area.
Best way to stay healthy?
Avoiding mosquito bites remains a high priority. Most travellers to southern resorts have access to rooms with central air conditioning and intact window screens, and hang out by a breezy beach where mosquitoes are less frequently encountered. Based on preliminary information, the areas of Brazil most affected by Zika at this time are in the poorer Northeastern areas of the country, and in the poorer neighbourhoods of Rio de Janeiro. This suggests that additional socioeconomic factors are at play, as was shown in a study with Dengue Fever.
If I'm travelling to South America, what precautions should we take?
All of the same advice that we give at home for the prevention of West Nile virus during the summer applies.
If I'm pregnant should I still go?
If someone is pregnant in their first trimester, and is not staying in high-end accommodation, then delaying the trip until later in the pregnancy or after the pregnancy might be justified.
We should be careful not to overreact and disrupt previous plans to what is still a low-risk event. (Remember how disruptive SARS was to Canadian tourism, despite a very low-risk to visitors?)
What are the risks in North America?
There are 22.7 million Americans living in areas of the U.S. where there could be year-round Zika transmission. But keep in mind the huge difference between the impact of another mosquito-transmitted virus -- dengue fever -- as shown by a study comparing Laredo, Texas, and Nuevo Laredo, Mexico. These two cities have an identical climate and straddle the Rio Grande River that forms the border between the two. However, the socioeconomic circumstances on each side of the border are very different.
Here's the surprise: even though Laredo, Texas had a higher concentration of dengue-infected mosquitos, the rate of recent infections on the U.S. side of the border was only 1.3%, while the rate on the Mexican side of the border was a whopping 16%. The biggest factor favouring the low rate of cases on the U.S. side was the availability of air conditioning.
The authors of the CDC study concluded that the "Texas Lifestyle" provides significant protection against a range of mosquito-transmitted diseases, and went on to say that despite climate change fostering an increasing global reach of mosquito-transmitted diseases into the U.S. (and perhaps the southern reaches of Canada one day), there may not be so many cases in the developed countries after all.
Dr. Neil Rau is a Medical Microbiologist; Assistant Professor, at the University of Toronto; medical director of Infection Prevention and Control with Halton Healthcare, and a consultant for CTV News as the Infectious Diseases Specialist.