As many as 400,000 Canadians suffer from Chronic Fatigue Syndrome, or Myalgic Encephalomyelitis. But according to a federal review, their condition is all in their minds.
Canada's largest scientific funding agency recently decided that ME/CFS is not deserving of research funding because it is not a legitimate disease, and more likely made up by patients.
That has infuriated patients such as Vancouver's Jasmine Sanchez-Ziller. For the past decade, the once athletic 25-year-old has been losing energy, leaving her housebound and mostly bedridden.
Sanchez-Ziller first started feeling ill in 2006, and kept getting worse. By 2008, she was so tired, she had to drop out of university. By 2010, she needed a wheelchair to get around, too tired to walk. By 2013 she was bed-bound.
It took Sanchez-Ziller's family more than five years to find her a diagnosis, in part because she had a gradual onset on the condition, rather than a more sudden onset of fatigue, which is more common.
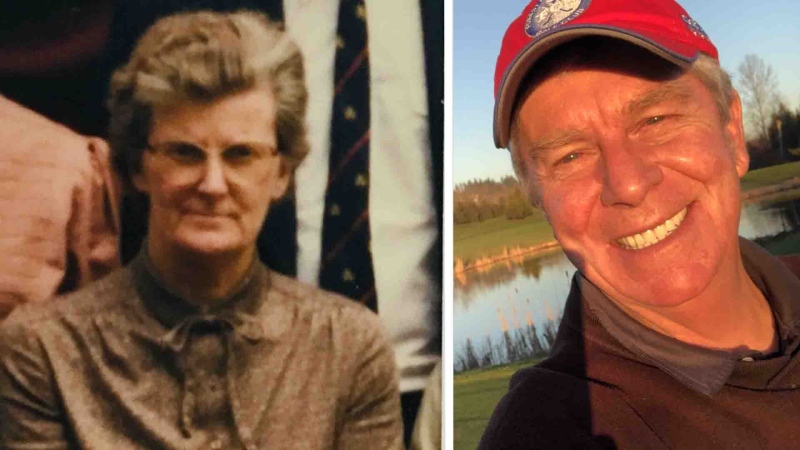
Jasmine's mother, Elizabeth, says she feels like she is losing the daughter she once knew.
"Her 20s are clicking by and this illness has just abducted her," she says.
Because the illness is so little understood, families like Sanchez's have called for more research funding.
In March, the Canadian Institute of Health Research (CIHR) agreed and asked scientists to submit proposals for up to $600,000 in funding to study ME/CFS. It then used an independent panel of experts in the field to evaluate the submitted applications.
A team of Canadian ME/CFS specialists submitted a proposal for that grant, with the aim of creating a research network, establishing standards of care for CFS patients, and educating doctors and other clinicians.
But their proposal - the only one from CFS researchers -- was rejected. The reason? The reviewers felt "there is no evidence that Chronic Fatigue Syndrome is a disease." It also said there was evidence that "psychosocial factors" are "both a cause and perpetuating factor for CFS."
In other words, ME/CFS is likely all in sufferers' heads.
Elizabeth Sanchez says she knows her daughter's illness is not imaginary.
"I see her deprived of her own life It makes me very sad and very angry. And if I could, wish this illness on those people, I would, just so they could know it is real," she says.
CFS patients and their families are furious with the decision, saying the review was based on outdated information, not the more recent research that shows that CFS is legitimate.
"It is a bit demoralizing," Sanchez said. "And it feels if it starts there, it is going to trickle down. There is no way to expect for doctors or other people in our lives to take it seriously if the researchers aren't even taking it seriously."
In a statement to CTV News, CIHR said it had “recognized the research gaps that will ultimately lead to better treatments for ME/CFS, and that building “appropriate research capacity” has been identified as key priorities.
They added that CIHR doesn’t review applications, and expresses no opinion about their quality. “CIHR’s role is to recruit external peers from the health sciences community and instruct them in peer review principles and procedures.”
CIHR said it is “actively discussing” how to address research gaps in ME/CFS, both “nationally and with international partnerships.”
Dr. Alison Bested is one of few Canadian specialists in the disorder and says the proposal response demeans patients by telling them their illness is in their heads.
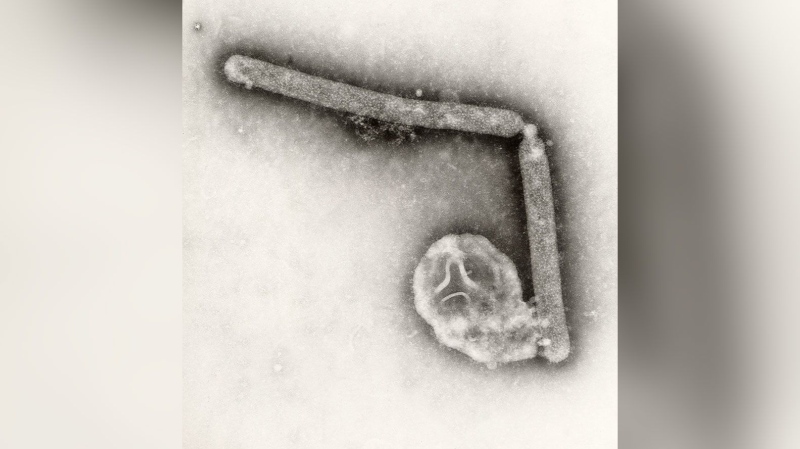
"We know for sure it is a physical illness that has a huge impact on the brain, the muscles, heart and the mitochondria," she said.
"The patients are in essence, in a resting state, they’re almost like in hibernation. Their bodies cannot produce the energy it needs,” Bested added.
Surprisingly, the federal government rejection may have actually helped the cause of CFS patients. These once-invisible patients, too tired to fight, are coming out from the shadows, forming groups using social media to push for recognition and research.
"This decisions means that patients are even further way from any hope of getting out of this terrible illness and it just puts us further behind."
Patient advocates are now going straight to the federal minister of health asking her to overturn the funding rejection and create a national research group.
"What needs to happen next is that the minister of health, Jane Philpott, needs to meet with our community she needs to meet with patient activists and advocates and doctors and researchers," says Dr. Bested.
Sanchez says she hopes to see an end to outdated thinking about CFS.
"The ignorance is having a severe impact on the lives of hundreds of thousands of people in this country and it is time for that to end," she said. "It is time for things to change."
With a report from CTV medical specialist Avis Favaro and producer Elizabeth St. Philip