Physicians have long been told that a child’s body mass index is the best way to measure obesity and related wellness issues.
But a group of Canadian researchers says that using only BMI, which measures weight against height, may actually underestimate disease severity in some cases and overestimate health risks in others.
The new study, called the Canadian Pediatric Weight Management Registry (CANPWR), suggests that a more holistic tool called the Edmonton Obesity Staging System for Pediatrics (EOSS-P) is better to assess a patient’s overall health and inform treatment options. The research, led by McMaster University in Hamilton, Ont., was published Tuesday in The Lancet Child & Adolescent Health journal.
“The clinical staging system definitely provides more information than BMI,” principal investigator Katherine Morrison, professor at McMaster’s department of pediatrics and co-director of the Centre for Metabolism, Obesity and Diabetes Research, said in a phone interview with CTVNews.ca.
The research shows that it may not be accurate to assume a patient with the most severe level of obesity based on BMI has the most severe health issues. In fact, some patients with the least severe BMI measures actually had moderate to severe health issues.
“You would miss those if you were only basing your practice plan on BMI,” said Morrison.
The new tool particularly stands apart for identifying mental health issues, which Morrison said were “pretty even across all of the body-size categories.”
The EOSS for pediatrics is adapted from the adult-oriented tool of the same name developed in Edmonton, Alta., which has been used successfully to determine the type and intensity of obesity treatment received by adults. The tool was adapted to account for children and adolescent concerns, including school, relationships with peers, and bullying. The new McMaster-led study used the tool with 847 children and adolescents who were enrolled in 10 different weight management programs across the country.
“The paediatric version has not yet been validated but seems to have reasonable face validity,” writes Australian paediatrician Louise A. Baur in a commentary on the new research.
The EOSS for pediatrics assigns a score of 0 to 3, based on severity, for four different subcategories of health risk:
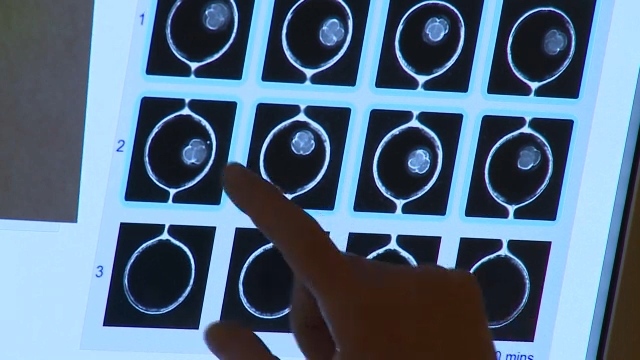
1. Metabolic (issues including dyslipidemia, type 2 diabetes and fatty liver disease)
2. Mechanical (issues including sleep apnea and orthopedic abnormalities)
3. Mental health (issues including anxiety and depression)
4. Social milieu (issues including low household income and bullying)
Participants in the highest BMI category had the greatest mechanical and social health risks. But the study’s main finding is that metabolic and mental health risks were comparable across BMI measures. Even children and adolescents with the lowest BMI had similar risks in those subcategories as those with higher BMI measures.
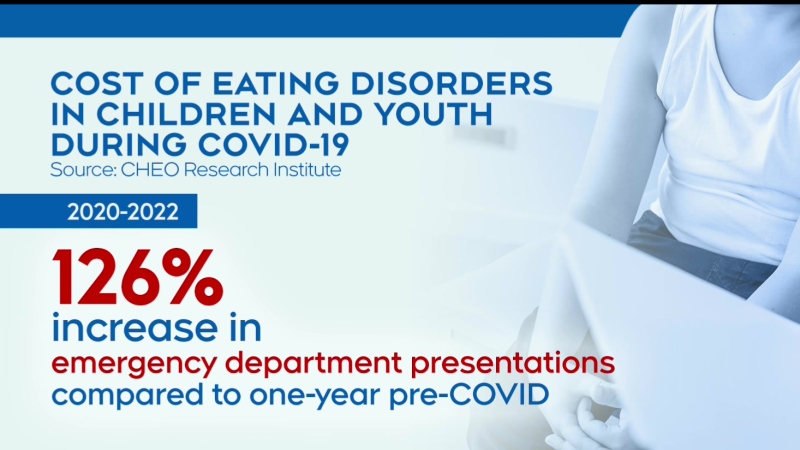
Obesity in children and adolescents is a global health risk, and though the rates have stabilized in Canada, Morrison said there is still much work to be done.
“They have stabilized at a pretty high level,” she said, noting that almost 1 in 3 children are obese. “At least it’s not going up. Our next job is to help it go down.”