A new review of patients in the Netherlands is shedding light on the controversial practice of euthanasia or assisted suicide among patients with psychiatric disorders, as the practice is increasing in certain jurisdictions. The review comes at a time when the Canadian government is crafting new legislation to address euthanasia in this country.
The review, published Wednesday in the journal JAMA Psychiatry, looked at 66 cases of euthanasia or assisted suicide (EAS) among patients with psychiatric disorders. The cases were from 2011 to 2014.
The new review found that in most of the 66 psychiatric EAS cases, the patients had chronic, severe conditions, with histories of attempted suicides or hospitalizations.
Dr. Scott Kim, the study's lead author, said the review is the first of its kind to provide a snapshot of how EAS cases are dealt with by physicians.
"For the first time, it provides a more fine-grained picture -- (rather) than mere quantitative data on reporting rates, etc. -- of what is happening when patients suffering from psychiatric disorders are euthanized or given lethal doses of medications for ingestion under the Dutch system," Kim, a psychiatrist and bioethicist at the National Institutes of Health, told CTV News in an email.
EAS has been practised in the Netherlands for decades, however formal legislation was only enacted in 2002. Although the numbers remain small, psychiatric EAS is becoming more frequent, the review authors note.
The researchers who wrote the review cite a Dutch study from 1997 that estimated the number of psychiatric EAS cases was between two and five. In 2013, there were 42 reported psychiatric EAS cases, the authors say.
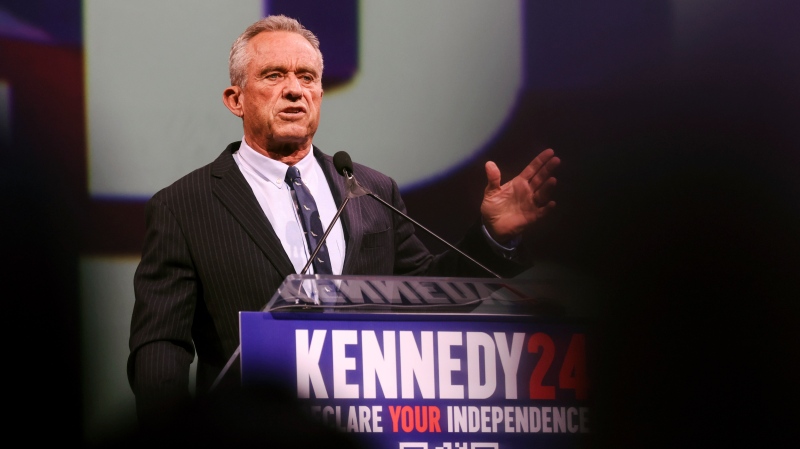
The review comes as the Canadian government crafts doctor-assisted death legislation. In January, the Supreme Court of Canada granted the federal government a four-month extension to come up with laws outlining assisted suicide and euthanasia in Canada. It remains to be seen whether mental illness will be included in the criteria.
Doctor-assisted suicide is legal to varying degrees in five U.S. states. However, none make it available to those with mental illness.
Majority of patients had depressive disorders
The study found that most of the 66 patients had more than one psychiatric condition, and depressive disorders were the primary issue in 55 per cent of those cases.
Other conditions observed in the patients included psychosis (26 per cent), PTSD or anxiety (42 per cent), and cognitive impairment (6 per cent). Eating disorders, as well as prolonged grief and autism were also observed.
The review found that 41 per cent of the patients had a psychiatric history spanning between 11 and 30 years, and in 27 per cent of the patients, the history exceeded 30 years. It also found that 58 per cent of the patients had at least one other illness, including cancer, heart disease or diabetes.
In 56 per cent of the case reports, there was mention of the patients' social isolation or loneliness.
The researchers found the following characteristics among the 66 patients:
- 70 per cent were women;
- 52 per cent had attempted suicide;
- 80 per cent had been hospitalized for psychiatric reasons;
Treatment and refusal
The study noted that patients with difficult-to-treat depression had sought different types of therapy, including electroconvulsive therapy and deep brain stimulation.
However, in one EAS case, a woman in her 70s without health problems had decided, with her husband, that they would not live without each other. After her husband died, she lived a life described as a "living hell" that was "meaningless."
A consultant reported that this woman "did not feel depressed at all. She ate, drank and slept well. She followed the news and undertook activities."
The review found that 21 patients had been refused EAS at some point, but in three cases the physicians later changed their mind and performed EAS. The remaining 18 patients had physicians who were new to them perform EAS.
In 41 per cent of the cases the physician performing EAS was a psychiatrist, but in the rest of the cases it was usually a general practitioner, the review found.
Consultation with other doctors was "extensive, but in 11 per cent of the cases, there was no independent psychiatric input. In 24 per cent of the cases, there were disagreements among the physicians.
Kim said the difficulty arises from the fact that the Dutch system relies on physician judgement to implement "fairly broad and vague rules."
He said that while the assessment of most terminal illnesses does not involve a lot of "physician discretion," and doctors can be "fairly sure" what the eventual outcome for the patient will be, psychiatric conditions are less clear.
"Physicians must make tricky clinical determinations … without the help of a robust evidence base," said Kim.
"There is no evidence base to operationalize 'unbearable suffering,' there are no prospective studies of decision-making capacity in persons seeking EAS for psychiatric reasons, and the prognosis of patients labeled as 'treatment-resistant depression' varies considerably, depending on the population and the kind of treatments they receive."
The review comes just days after the family of a 37-year-old woman, who received doctor-assisted suicide in 2010, went public in an attempt to bring light to the issue.
According to Life Site News, Lotte and Sophie Nys said their daughter, Tine, told them on Christmas Eve in 2009 that she wanted to seek euthanasia. Tine's relationship with her boyfriend crumbled and, according to her parents, psychological issues from her youth resurfaced.
Her parents said that Tine Nys then "shopped around" for doctors, eventually finding one to perform the euthanasia, and two others, including a psychiatrist, to confirm that the criteria of the law had been met.
However, her parents said the doctors did not confer together about the state of their daughter's health and she received a new diagnosis -- that she had autism -- two months before her death, in order to justify the procedure.
The family said they have not received an answer as to why no new medical help was offered after the new diagnosis, and they have lodged a judicial complaint against the three doctors.
'Serious concerns'
A separate editorial says the review of the Dutch cases raises "serious concerns."
Dr. Paul Appelbaum, of the New York State Psychiatric Institute, says there are particular concerns that come with the practice of EAS in psychiatric patients.
He notes that, in many such patients, a desire to die is often part of their disorder. As well, their response to treatment is less certain, meaning it's "much more difficult" for doctors to assess patients’ competence to decide to end their lives.
Appelbaum points to many troubling trends observed in the Dutch data, including the finding that 56 per cent of the cases included reports in which "social isolation or loneliness was important enough to be mentioned."
This "evokes the concern that (EAS) served as a substitute for effective psychosocial intervention and support," he said.
He also noted that it was also troubling that, in 12 per cent of cases, the "psychiatrist involved believed that the criteria for EAS were not met, but assisted death took place anyway."
There are several moral implications to consider as well, including the concern that psychiatrists may conclude from the legalization of EAS that it is acceptable to give up on treating some patients, he said.
Appelbaum noted, however, that it is important to keep in mind the limitation of the Dutch data.
In particular, the available sample did not reflect all cases involving psychiatric disorders. As well, the cases only included cases where EAS took place, which does not allow any conclusions to be drawn about the effectiveness of the screening process.
Two options
Trudo Lemmens, a professor at the University of Toronto who specializes in bioethics, told CTV News that two main options are on the table in Canada.
The first proposal would rely on the assessment of a physician, with secondary verification coming from another physician.
However, Lemmens said this option leaves the door to potential "doctor shopping."
The second proposal, he says, has more "stringent criteria" and narrows down the availability of doctor-assisted suicide to solely those with "particular" medical issues, and would exclude those with conditions like autism.
Lemmens said it would also involve a second review, involving an "independent panel" to make sure the criteria are met.
"The second proposal is, in my view, superior and provides safeguards that the Belgian system doesn't have," said Lemmens.
Lemmens suggested that the issues with those systems could be remedied by having mental assessments done by more than one physician, and also forcing patients to go through a "cooling-off period to make sure they don't change their mind."
Tara Brousseau-Snider, executive direct of the Mood Disorders Association of Manitoba, said she is concerned about the potential of Canada offering doctor-assisted suicide to those with mental illness.
She said a woman with severe depression came into the Winnipeg centre just months ago and told a counsellor that she wanted to end her life.
"I find this is very alarming, very worrisome because people, through different avenues, find a different way of life and nobody needs to sit with depression and be miserable all through their lives. There are options; there are supports available," said Brousseau-Snider.
With files from CTV News' Medical Correspondent Avis Favaro and producer Elizabeth St. Philip