Last week, a small U.S. biotech firm announced that its supply of experimental Ebola drug ZMapp had run out.
ZMapp was given to two American missionaries who recovered from Ebola, although it’s not known whether the drug, or the standard of care in an Atlanta hospital, was responsible for their survival.
The maker of ZMapp, San Diego-based Mapp Biopharmaceutical, told the New York Times earlier this month that it has been “overwhelmed” with requests for more doses. The company said it’s in discussions with the U.S. Food and Drug Administration to find “the right path” to produce the drug as quickly as safely as possible.
Although no timeline was given, health officials in western African countries affected by the Ebola outbreak have said that it could take months before ZMapp and other experimental therapies could be used on Ebola patients there.
Mapp Biopharmaceutical is a small firm with only nine employees, according to reports. It only had a small amount of ZMapp available because safety studies in humans were not being planned for at least another year.
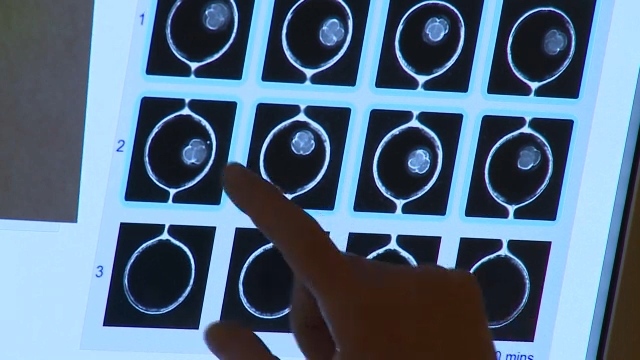
Because the drug is generated in tobacco plants that have been genetically engineered to produce the monoclonal antibodies needed to target the Ebola virus, production also depends on the tobacco company responsible for those plants.
Supplies of other experimental Ebola treatments are also “extremely limited,” the World Health Organization said Thursday.
In two weeks, the WHO will hold a consultation in Geneva in an effort to identify the most promising experimental Ebola treatments and vaccines. More than 20 experts from West Africa are expected to attend.
“Possible ways to ramp up production of the most promising products will also be explored,” the WHO said.
Promising results, but no proof it works
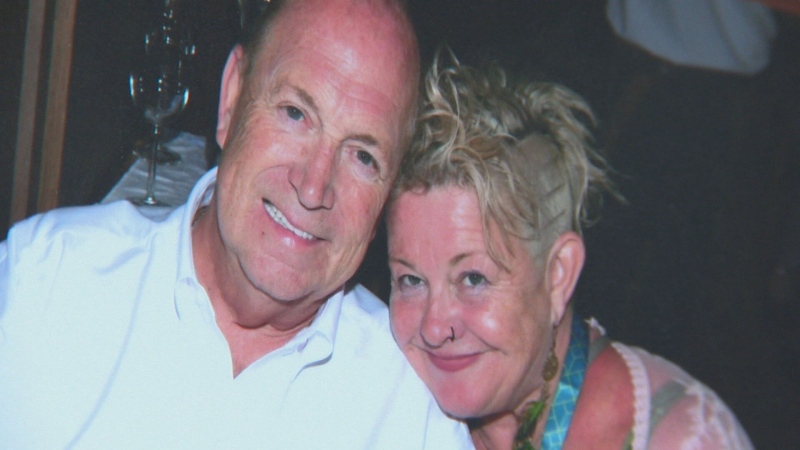
ZMapp, which had never been clinically tested on humans, was given to Dr. Kent Brantly, 33, and nurse Nancy Writebol, 59, both of whom were infected with the Ebola virus while working at a missionary clinic in Liberia.
After nearly three weeks of treatment, they have now been discharged from an Atlanta hospital.
Another doctor who was given the drug is still in serious condition, but has “improved somewhat,” the WHO said. A Spanish missionary priest who was reported to have received the experimental treatment died.
Commenting on the controversy brewing over the use of experimental Ebola therapies, Dr. Neil Rau, a Canadian infectious disease specialist, said “there is no question” that some people will compare their use now with the uneven distribution of life-saving drugs at the height of the HIV/AIDS crisis.
“The difference here is that we don’t know that we have a treatment that works,” he told CTV News Channel Thursday.
Rau said it’s difficult to advocate for wider use of ZMapp and other potential Ebola therapies because they haven’t been rigorously tested.
An editorial published in the medical journal The Lancet Thursday calls on researchers and health authorities to ensure that experimental Ebola drugs are “distributed fairly, and in the context of randomized controlled trials.”
In The Lancet piece, leading bioethicists say that patients selected to receive experimental drugs “must not be limited to well-off or well-connected patients – including health care professionals.”
Canadian connection
ZMapp uses a mix of three monoclonal antibodies to attack the Ebola virus, and two of those antibodies are the result of Canadian research by scientists at the National Microbiology Laboratory.
The drug itself was co-created by Mapp Biopharmaceutical, based in San Diego, and Defyrus Inc., which is based in Toronto.
Dr. Jeffrey Turner, president of Defyrus, said his company worked on the “front end” of the drug, testing the monoclonal antibodies in animal models to predict how they will work.
“We can tell you that in all of the studies that we’ve developed here in Canada and in the United States on animal models … the effects are dramatic, that the animals can survive lethal infections of the Ebola virus,” he told CTV News.
Turner said he hopes to continue preclinical work on the drug, but it’s been difficult because it takes months to produce ZMapp.
“We’re hoping by the end of the year that sufficient material will be available so we can continue to do the preclinical work,” he said.
With a report by CTV News' Medical Specialist Avis Favaro and Senior Producer Elizabeth St. Philip