After her son caught COVID-19 earlier this year, Jessica Botelho said she was looking forward to his annual checkup. While three-year-old Jaxson has since recovered from his high fever and upset stomach, Botelho said she wanted to make sure he wasn't suffering from any long-term complications.
But when she tried booking an appointment at her son's clinic in August, she was told the earliest appointment she could get was in November, she said.
“[The secretary] basically said people are waiting three to six months for an appointment,” she told CTVNews.ca in a telephone interview on Thursday. “Their excuse for everything that's been going on is COVID.”
Botelho is one of several parents who wrote to CTVNews.ca about their difficulties with booking doctors' appointments for their children over the last few months. The emailed responses have not all been independently verified.
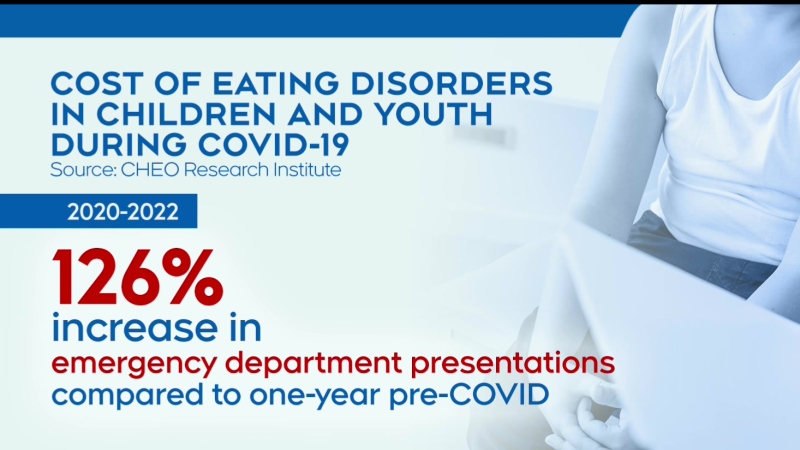
An increase in cases of respiratory syncytial virus (RSV) among children is leaving pediatric hospitals across Canada overwhelmed by the surge of new patients. In addition to RSV, cases of COVID-19 and the flu are also contributing to an increase in viral infections at hospitals, resulting in what experts are calling a “multi-demic.”
This prompted federal health officials to urge Canadians to wear face masks while indoors. During a COVID-19 update on Thursday, Canada's Chief Public Health Officer Dr. Theresa Tam said multiple layers of protection will be crucial to reduce the impact of a fall surge of COVID-19, RSV and influenza cases on hospitals.
The rise in cases of RSV and influenza in children across the country is “putting extreme pressure on both children's hospitals and community-based health-care providers,” the Canadian Paediatric Society (CPS) wrote in a statement to CTVNews.ca on Nov. 14.
“Unfortunately, that means wait times are getting longer,” the statement reads.
Despite the difficult circumstances, the CPS said pediatricians are working hard to continue to provide care to patients.
“While we can't speak to every situation, we believe the majority of paediatricians never stopped seeing ill children in person,” the organization wrote. “Many have set aside specific times of day for symptomatic or feverish children in order to protect their other patients.”
Botelho said the clinic her son attends only sees patients who are symptomatic during a one-hour period each day, from Monday to Friday. During this time, parents can walk in with their sick children without an appointment. If it's a medical emergency, they are advised to go to straight to the nearest emergency department for assistance.

Botelho said she's unsure whether allowing symptomatic patients in the clinic at a specific time will actually help curb transmission. This is because children under the age of two are not required to wear masks in the clinic.
“It doesn't really make a difference because if they're under the age of two, they don't wear a mask,” said the Toronto-based mother of two. “So I can still go in there with my one-year-old and [he can] end up getting sick.”
With the ongoing transmission of COVID-19, as well as RSV and influenza, Botelho said she is very worried about the chances of her children getting sick. Added to that pressure is the uncertainty of whether they will be able to see a doctor within a reasonable amount of time if they do get sick, she said.
“It's frustrating because you know they have to get sick and build their immune system, but the stuff that's out there right now is putting kids in hospital and that's my big fear,” she said. “What if he was sick now, am I going to wait months for an appointment?
“All we want is to see the doctor to make sure our kids are healthy.”
LACK OF EXPOSURE CONTRIBUTING TO LOW IMMUNITY
When her two-and-a-half-year-old daughter caught pneumonia last month, Tanya Copley said she also struggled to book a doctor's appointment. Based in Montreal, Copley said her daughter's pediatrician is currently on maternity leave.
With limited availability at her daughter's clinic, Copley had to rely on doctors at other facilities when scheduling an appointment for her daughter. Using the Centre Up and Rendez-vous santé Québec online platforms, she tried booking an appointment for her daughter but due to demand, spots were quickly filled.
“Almost every minute I was refreshing my page on the website and I couldn't find anything,” she told CTVNews.ca in a telephone interview on Sunday. “It's just a nightmare, especially when you know your child is sick with something like a respiratory illness.”
After a few days of searching, Copley was able to schedule an appointment on Oct. 22 at the Centre Médicale Mieux-Être in Montreal, a 40-minute drive from where she lives. She said she believes part of the reason behind the increased demand for pediatric appointments is parents and daycares “letting their guard down.”
“Before, the second they coughed, the daycare would call you up and tell you to come pick up your child, they're sick,” she said. “Now, suddenly everyone is catching something and all their little friends catch it too.”

A lack of exposure to respiratory illnesses is also contributing to low immunity among children, said Deputy Chief Public Health Officer Dr. Howard Njoo. In the federal government's COVID-19 update on Thursday, he said immunity to RSV and other respiratory viruses is particularly low among children who have largely remained in confinement over the past two years due to COVID-19 public health measures.
According to the CPS, the ongoing shortage of children's pain and fever medications, such as Tylenol and Advil, also plays a role in the increased demand for appointments within Canada's health-care system.
“It has definitely been a rollercoaster trying to decide when your child is sick enough or when you have attempted all other options for long enough before going to go to the ER,” Copley wrote in an email to CTVNews.ca on Thursday.
Dr. Allan Grill, chief of family medicine at Markham Stouffville Hospital, spoke to CTV News Channel on Sunday. For parents trying to decide whether to take their children to an emergency room, he said to look for symptoms such as difficulty breathing, struggles with eating or drinking and chest pains.
After visiting the clinic, Copley said her daughter was given antibiotics to treat her pneumonia and has since recovered. Going forward, she might rethink her strategy when trying to book a doctor's appointment for her daughter, she said.
“If they have a fever, I might try looking for something right away rather than waiting two to three days,” she said. “Or calling up the pediatric clinic rather than just expecting them to say you have to book online.”
PARENTS LEFT FEELING 'STUCK'
On Thanksgiving Monday, Stephanie Paradis said, her eight-year-old son woke up with a fever of about 38.9 C (102 F) for the third day in a row, along with a sore throat and cough. At that point, she started to consider taking him to their family doctor's after hours clinic.
But after visiting the clinic's website, she saw they were not accepting patients with symptoms such as fever, chills, muscle aches or cough, she said.
“I've never seen that before,” she told CTVNews.ca in a telephone interview on Thursday. “I can honestly say I was a bit surprised, I felt very stuck.”
Instead, Paradis took her son to Guelph General Hospital, where they waited a few hours in the emergency room for a physician, she said. After doing X-rays, her son was given antibiotics and after a week, his condition improved.
While her son got the help he needed, Paradis said she felt as though the situation could have been handled by her family doctor.
“We felt like we had no other option,” Paradis said about her family's decision to visit an emergency room. “I feel like people are being redirected [to hospitals] because family doctors are screening patients. It's not helping our health-care workers and hospitals that are already overwhelmed.”

Since then, Paradis said, her family doctor's clinic has changed its policy. Now, patients with symptoms such as fever, chills, muscle aches or cough are required to test negative using a COVID-19 rapid antigen test at home before visiting.
Despite this, Paradis said she still worries about whether her son will be able to see a doctor so soon if he were to get sick again.
“It doesn't make me feel like he's safe if he gets sick again,” she said. “It's very worrisome.”
The CPS is asking Canadians over six months of age to get their annual flu shots as soon as possible and ensure they are up-to-date on their immunizations, which includes COVID-19 vaccines.
“This, along with staying home when unwell and masking in public spaces, works to slow the transmission of viral illnesses and help keep children healthy,” a statement from the CPS reads. “We ask everyone to do their part to relieve pressures on the children's health-care system.”
CUTS TO VIRTUAL CARE BILLING ‘COULD NOT COME AT A WORSE TIME’: DOCTOR
Instead of meeting with doctors in person, many patients have had the option to speak with physicians virtually throughout the pandemic. However, as of Dec. 1, the province of Ontario will see changes to the funding framework of its virtual care program set out in the Physician Services Agreement. As part of Ontario’s updated health insurance plan, doctors who receive funding for limited virtual care will see a drop in the amount of money they receive per patient.
Limited virtual care refers to health care that a patient receives from someone who is not their regular physician, or to whom they have not been referred. This involves services provided by doctors at virtual pediatric clinics that operate on an ad-hoc basis, such as KixCare. The 24/7 virtual clinic is available to children across Ontario.
Doctors providing limited virtual care services by video will receive $20 per patient and $15 per patient for services provided by telephone, according to an updated schedule of benefits from the Ontario Ministry of Health. This represents a significant drop in funding, said Dr. Aviva Lowe, a Toronto-based pediatrician who works for KixCare.
“It’s at least a 75 per cent cut for virtual care for pediatricians,” she told CTVNews.ca in a telephone interview on Tuesday. “There’s been a significant funding cut to the point where, especially for pediatricians, that type of service is effectively being defunded to the point of lack of viability.
“It will cease to exist, for the most part.”
In a statement to CTVNews.ca on Tuesday, Ontario Ministry of Health spokesperson Bill Campbell said “virtual care is intended to compliment in-person care, not replace it.
“This approach has resulted in meaningful changes for virtual care that ensures a positive patient-physician relationship is fostered,” Campbell said.
These clinics help families see pediatricians within a timely fashion, Lowe said. Faced with the possibility of fewer clinical options as a result, families are likely to visit hospital emergency rooms for assistance instead, said Lowe, making it tougher to receive the care they need. Pediatric hospitals across Canada continue to be overwhelmed by a surge of patients as cases of RSV and the flu continue to rise.
“This defunding could not come at a worse time,” Lowe said. “It’s not the time to be cutting access to health-care options that currently are serving as a pressure valve on keeping non-emergent children out of the ERs.”
With files from The Canadian Press and CTVNews.ca’s Megan DeLaire and Natasha O’Neill