VANCOUVER - Brynessa Gradley's life changed just over a year ago when she scratched an itchy spot on her leg as she came out of the shower.
The 21-year-old Queen's University student, a native of West Vancouver, found a tiny mole ringed with reddened skin and decided to have it checked out at the campus clinic.
The clinic doctor referred Gradley to a dermatologist -- reluctantly because of her youth and lack of family skin cancer history. She says she also had to push the skin specialist to order a biopsy.
"I came back to Vancouver for the summer and received a phone call that I would need emergency surgery, without which the cancer would have spread throughout my body within a month," Gradley said Thursday.
Gradley was diagnosed with malignant melanoma, the deadliest form of skin cancer, which is expected to take 940 Canadian lives this year.
Canada's dermatologists, who are meeting in Vancouver this week, say skin cancer rates, including melanoma, are on the rise among young people just as the number of skin specialists is set to decline.
The Canadian Dermatology Association says Canadians born in the 1990s are two- to three-times more likely to get skin cancer in their lifetime, compared with those born in the 1960s -- one in six versus one in 20 for the older group.
The lifetime risk of melanoma for Canadian men now is one in 74, for women one in 90. By comparison, the lifetime risk for Americans in the 1930s was one in 1,500, the association says.
The association forecasts 75,100 Canadians will be diagnosed with non-malignant skin cancer this year, and 5,000 will learn they have melanoma.
Young people aged 15 to 29, especially women, seem to be contracting melanoma at alarming rates. It accounts for seven per cent of all new cancers found among young men, 11 per cent among young women, the association says.
The fair-skinned Gradley said she had never been sunburned but played a lot of outdoor sports as a teen and first used tanning beds at age 13.
She said she's lucky she got in to see a dermatologist fairly quickly.
"I received a very invasive surgery," said Gradley. "I was on crutches for three months and walked with a cane afterwards."
Wait times to see the skin specialists have doubled in the last five years to about 10 weeks, says Dr. Larry Warshawski, the association's outgoing president.
"Dermatologists themselves are striving to increase our capacity to see patients," the Vancouver-based doctor said. "Our problem right now is numbers. There are only about 650 dermatologists across the country right now."
The problem appears set to get worse. The association's most recent data shows a median age for Canadian dermatologists in the 50s, with 45 per cent set to retire within the next 10 years.
An aging population suggests the pressure for their services will increase in coming years.
Warshawski's successor as president, Dr. Yves Poulin, said his priority this year will be to lobby provincial governments to increase the limited number of residency spots for dermatologists to address the expected shortfall.
It can take 13 to 15 years to produce a dermatologist, including a five-year residency and optional fellowships of up to two years.
The association is also lobbying provincial governments to bar people under age 18 from using tanning beds.
Meanwhile, the association is focusing on public awareness.
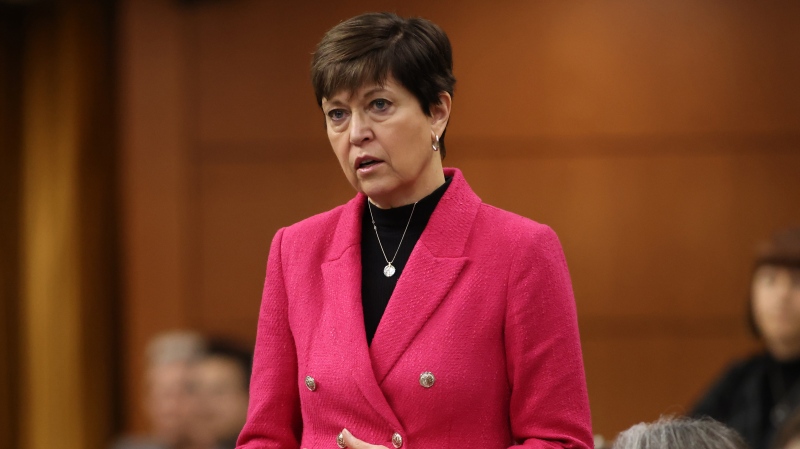
Member of Parliament Dona Cadman, who lost her husband Chuck to melanoma in 2005, sponsors an annual screening on Parliament Hill.
Cadman said she'd nagged her MP husband for months to have a dodgy mole checked out but he didn't until it was red-flagged at another screening event.
"He finally took it serious after going to the clinic," Cadman said. "In the end maybe those few months might have saved his life."
A survey conducted in May for the association found more than 90 per cent Canadians can recognize what a potential melanoma looks like.
But far fewer knew the risks factors, such as having light skin or suffering sun burns, said Dr. Cheryl Rosen, head of the association's sun-awareness program.
Canadians also rarely examine themselves for early signs of skin cancer.
Surprisingly, many survey respondents were ready to ignore protective measures in their quest for a tan, she said.
"There were a large number of people who would not avoid a tan even if they knew it would decrease their risk of developing skin cancer," said Rosen.
Among many people tans are still seen as a sign of good health, something Rosen wants to "denormalize."
"There is a culture of being tanned is being beautiful," Gradley added.
Dermatologists are also concerned about recent promotion of brief sun exposure to gain the benefits of vitamin D.
"There are far safer ways to get your vitamin D than going out in the sun," said Rosen. "A vitamin D tablet or capsule works just as well as sun exposure."
She noted vitamin D conversion can be affected by the use of sunscreens and other factors such as age and skin colour.
Gradley said a series of fully body scans have confirmed her cancer is in remission but she must go for twice-yearly checkups for the rest of her life.