A large U.S. study links an increased risk for developing dementia to high and prolonged use of common medications, including popular antihistamines, sleep remedies and older anti-depressants.
The study, published Monday in the journal JAMA Internal Medicine, is the first study to show a dose-response relationship, linking higher and longer use of anticholinergic medications to an increased risk for developing dementia, including Alzheimer's disease, according to its authors.
The study is also the first to suggest dementia risk linked to the medications may be irreversible, even after patients stop taking the drugs in question.
Anticholinergic medications include a range of popular drugs, including non-prescription medications like diphenhydramine, commonly known as Benadryl. Other medications containing anticholinergic substances include the anti-depressant Sinequan, certain first-generation antihistamines, and Ditropan, a drug used to treat urinary and bladder problems.
The study estimates that patients taking at least 10 mg/day of the anti-depressant doxepin, 4mg/day of the antihistamine chlorpheniramine, or 5 mg/day of oxybutynin (to treat bladder infections) for more than three years would be at greater risk for developing dementia.
Lead author Dr. Shelly Gray, from the University of Washington, said that older patients should know the risks associated with these medications.
"Older adults should be aware that many medications – including some available without a prescription, such as over-the-counter sleep aids – have strong anticholinergic effects," Gray said in a statement.
Gray added that older adults should tell their doctors about all of the over-the-counter medications they use. And she said health-care providers should regularly review their elderly patients' drug schedules to reduce the amount of anticholinergic medications consumed.
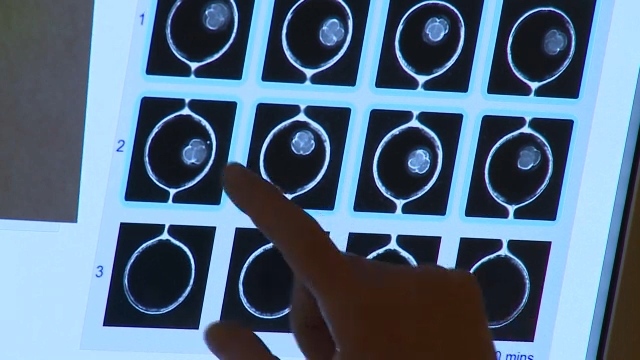
The study examined pharmacy data from 3,434 participants over the age of 64 with no prior diagnosis of dementia. The patients' data was examined to determine the level of anticholinergic medications they consumed. The data was also examined to determine how many patients went on to develop dementia or Alzheimer's.
After about seven years of follow-up, the researchers found that 637 participants (18.5 per cent) had developed Alzheimer’s disease, and 160 (4.6 per cent) had developed other forms of dementia. By comparison, about 15 per cent of Canadians 65 and older live with some form of dementia, according to the Alzheimer Society of Canada.
“Our findings suggest that a person taking an anticholinergic, such as oxybutynin chloride, 5 mg/d, ordoxepin hydrochloride, 10mg/d, for more than 3 years would have a greater risk for dementia,” the authors of the study wrote in their conclusions. “Prescribers should be aware of this potential association when considering anticholinergics for their older patients and should consider alternatives when possible.”