Sharing needles isn’t the only way to spread HIV among drug users, according to Ontario researchers who have discovered a new method of transmission involving the equipment used to prepare the drugs before injection.
In two studies, published in the Journal of Acquired Immune Deficiency Syndromes (JAIDS) on Thursday, researchers from Lawson Health Research Institute and Western University in London, Ont., show that hygienic needle or syringe habits may not be enough to protect people who inject drugs.
From August 2016 to June 2017, the research team interviewed 119 injection drug users to learn more about their habits.
“We asked them how they inject and what they do,” Dr. Michael Silverman, chief of infectious diseases at Western University and an associate scientist at Lawson Health Research Institute, said in a video accompanying a press release.
Silverman said the majority of respondents revealed they shared cookers and filters, the materials used to prepare drugs such as hydromorph contin, or controlled-release hydromorphone – one of the most commonly injected opioids.
“In fact, 96 per cent of people who used hydromorph contin reused and did multiple washes with the drugs,” he said.
A “wash” is the mixture that results from dissolving drugs in water in a metal “cooker.” The wash is then drawn into a syringe using a filter.
As a result, the researchers found that those who shared equipment such as cookers and filters were 22 times more likely to contract HIV than those who didn’t, even if they didn’t share needles or syringes.
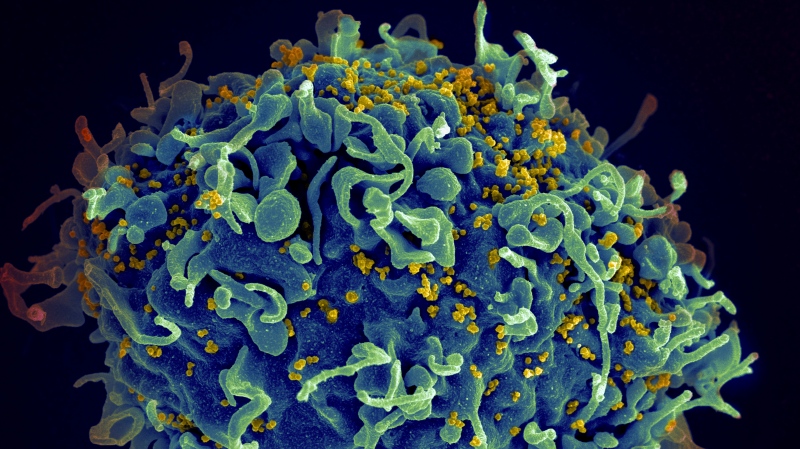
Furthermore, the academics discovered the type of drug – hydromorphone – that most users were injecting has unique properties, which allow the HIV virus to survive on the equipment.
“Controlled-release hydromorphone is expensive and difficult to dissolve. After the first wash, large amounts of the drug remain in the equipment which is then saved, shared or sold for future use,” Dr. Sharon Koivu, an associate scientist at Lawson Health Research Institute and an associate professor at Schulich Medicine & Dentistry, said.
“While people know not to share needles, some use their own needle multiple times allowing for contamination of the equipment.”
On average, the researchers said that 45 per cent of the drug remains in the equipment after the first wash.
“The slow-release properties in the drug can unfortunately stabilize the HIV virus,” Eric Arts, chair of the Department of Microbiology and Immunology at Schulich Medicine & Dentistry, said.
Developing a solution
Despite the discovery of another method of transmitting HIV, the researchers were encouraged by another one of their findings – an easy way to sterilize equipment for drug users.
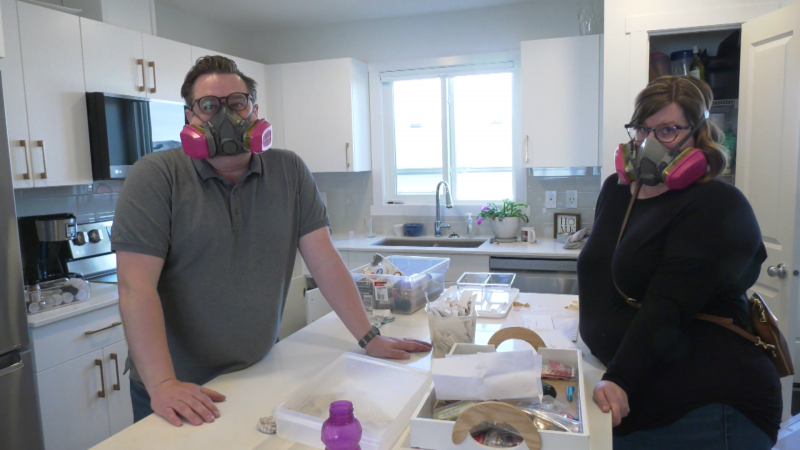
By heating the metal cooker with a cigarette lighter for approximately 10 seconds, or until the wash bubbles, the researchers were able to kill the virus on the cookers and filters.
“Nobody wants to be using their equipment in a way that puts them at risk. People want to be doing things that are as safe as possible, so understanding that if you heat your cooker to boiling for 10 seconds that can make a huge difference in your risk of getting an infection,” Koivu explained.
The researchers were also able to determine that heating the cooker didn’t change the drug concentration in the mixture, meaning users would be more likely to try it.
“If too much drug was released, it could lead to overdoses. If any drug was burnt off or lost, the intervention would not be accepted by persons who inject drugs,” Silverman said.
In partnership with several local community organizations, including the Middlesex-London Health Unit and Regional HIV/AIDS Connection, the research team launched the “Cook Your Wash” public health campaign to teach drug users how to sterilize their equipment and prevent the spread of HIV.
“The ‘Cook Your Wash’ campaign is one of the most exciting things to happen in our community,” Koivu said. “We learned from persons who inject drugs, took that information to the lab to develop a solution and then brought that solution back to the community in record time.”
Since the campaign was introduced, Silverman said that rates of new HIV cases have fallen dramatically in the London area.
“It wasn’t the sole reason for the reduction in HIV rates as other interventions were also introduced, but the timing suggests it was part of the solution,” he said.
The academics said they hope the studies will inform future research on HIV prevention and treatment.
“We hope our findings can be used to reduce the incidence of HIV transmissions even further and that, one day, society will be HIV free,” Silverman said.