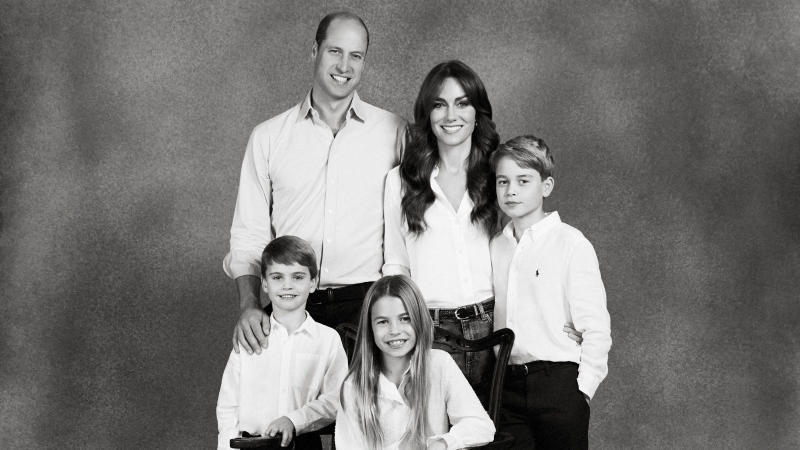
A treatment never before tried on a child in Canada has helped a young girl who was suffering from seizures several times every hour.
Andi Dreher’s seizures had steadily worsened during her first nine years of life. Various treatments, including brain surgery and an assortment of medications, were unable to reverse the pattern and bring peace to the girl from Kitchener, Ont.
“Everything helps in different pieces, but not one thing [has been] able to fix her,” Dreher’s mother Lori told CTV Toronto.
By this fall, Dreher was having 100 to 150 small seizures – she calls them “glitches” – on a daily basis and was no longer able to walk, use the washroom or even sit still on her own.
“She knows she has them … but she doesn’t really know that they’re happening,” Lori Dreher said.
“She wants to do things and be like everyone else, and she can’t.”
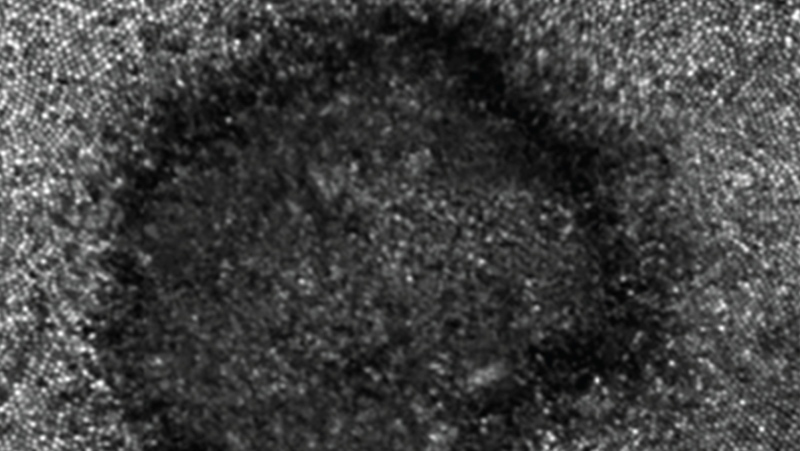
Doctors had been able to trace the seizures to a small part of Dreher’s brain, next to an unusual arrangement of blood vessels in her brain, which made surgery extremely risky.
Dreher ended up at The Hospital for Sick Children in Toronto, where doctors decided to try to treat her epilepsy with deep brain stimulation (DBS) – a Canadian first for a child with that condition, and a procedure believed to have been used on children only 40 times worldwide.
Experts were brought in from Toronto Western Hospital, which uses DBS to treat Parkinson’s disease, epilepsy and other conditions in adults. The procedure involves implanting an object similar to a pacemaker in the patient’s chest and using it to send electrical impulses to the brain.
Dreher’s parents will be able to use a handheld device to adjust the levels of electricity being sent to the brain.
Dr. George Ibrahim, a neurosurgeon who worked on Dreher, says the implant essentially allows for Dreher’s neural pathways to be remapped to achieve specific goals.
He said DBS made particular sense for Dreher because of her “unique brain structure” and the procedure’s ability to microtarget regions of the brain.
The surgery took place Oct. 1. It went well, with Dreher being allowed to go home within a few days.
Doctors say they won’t be able to tell with certainty whether DBS will provide Dreher with long-term relief for several months. However, a test they performed with the device during the surgery has them feeling optimistic.
“We were very encouraged that when we turned on the circuits in the surgery theatre, we saw some changes in her brain rhythms,” Ibrahim said.
Lori Dreher says her daughter’s seizures have become less frequent since the device was switched on for good last month.
“We have to be hopeful, because we’re running out of options,” she said.
Even if the implant does seem to make a difference, doctors will continue to monitor Dreher very closely to monitor how her brain adjusts to the electrical jolts – both because of the uniqueness of her case and because there is little existing long-term evidence about how children respond to deep brain stimulation as they grow and develop.
“We’re going to be following Andi very closely over the next several years to make sure that there are no unforeseen circumstances,” Ibrahim said.