Your gluten-free diet may, in fact, not be the reason your upset stomach, fatigue and headaches have gone away, says a recent study.
The researcher who first discovered evidence of non-celiac gluten insensitivity three years ago now says gluten is not always to blame for gastrointestinal and other symptoms reported by patients who do not have celiac disease.
Celiac disease is a medical condition that renders the body unable to absorb the proteins in wheat, barley and rye, which attack the digestive system and cause a variety of gastrointestinal and other symptoms.
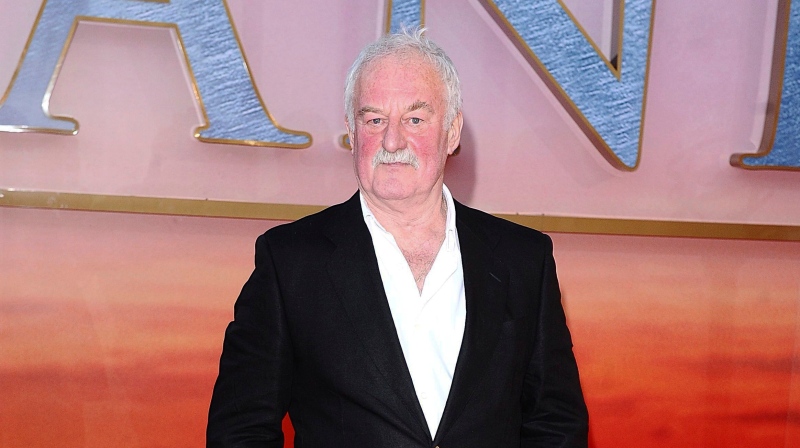
Prof. Peter Gibson, director of gastroenterology at Alfred Hospital in Melbourne, Australia first found evidence in 2011 that gluten triggered symptoms in non-celiacs. Despite the fact that it was a randomized, double-blinded study -- the most rigorous kind -- Gibson wanted to drill down on another question: What is really causing the improvement in symptoms when people stop eating wheat?
Gluten was often cited as the cause. However, fermentable, short-chain carbohydrates could be another culprit.
Known by the acronym FODMAP, these carbs are poorly absorbed by the small intestine.
The question for Gibson became whether people who feel unwell after eating wheat are having problems with the gluten content or the carbohydrate content.
His most recent study, published in the journal Gastroenterology, included 37 subjects who reported having non-celiac gluten sensitivity and irritable bowel syndrome, but who were negative for celiac disease.
They began with a two-week diet low in FODMAPs, and were then placed on a high-gluten diet (16 g of gluten per day), a low-gluten diet (2 g of gluten and 14 g of whey protein a day) or a control diet (16 g of whey protein a day) for one week.
All subjects were assessed for intestinal inflammation and other problems.
After a “wash-out period” of two weeks, 22 subjects spent three days either on the high-gluten diet, a diet of 16 grams of whey protein per day, or a control diet with no additional protein.
“In all participants, gastrointestinal symptoms consistently and significantly improved during reduced FODMAP intake, but significantly worsened to a similar degree when their diets included gluten or whey protein,” Gibson and his research team write in their study.
“Gluten-specific effects were observed in only eight per cent of participants.”
Gibson told the American Gastroenterological Association that the team attributed some of the worsening symptoms to the “nocebo” effect, such as the kind of symptoms people report from wind turbines and Wi-Fi.
“What the study has shown is that this entity of non-celiac gluten sensitivity as reported by patients may not exist,” Gibson told the agency. “There’s a possibility that gluten might cause problems while they are on a high FODMP diet, but that’s a question that we didn’t answer in this study.”
When asked what advice he would have for doctors with patients reporting having gastrointestinal symptoms, Gibson said they should first try a low-FODMAP diet.
“We would only restrict gluten in a small proportion of patients where we’re not winning and we have a strong belief that wheat is a cause of their symptoms.”