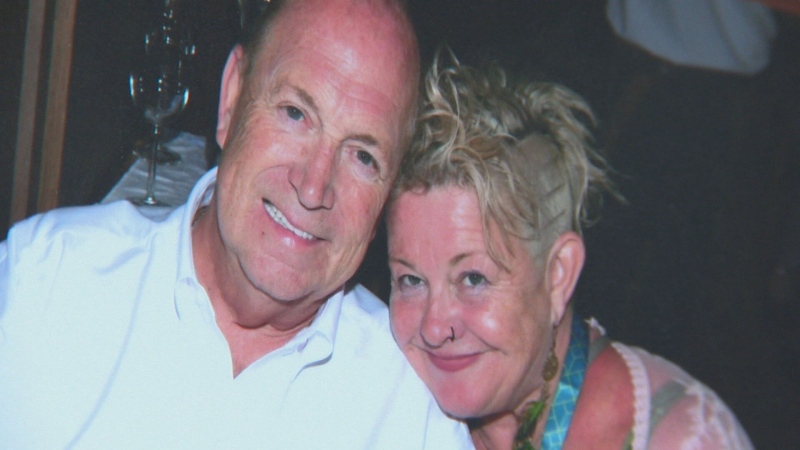
As a B.C. mother approaches the one-year anniversary of her son’s fatal fentanyl overdose, she says the federal government’s response to the ongoing crisis has been “dismal” and doesn’t take the problem seriously enough.
Brandon Jansen, 20, died last March while being treated for his addiction to fentanyl at a privately run facility in Powell River, B.C. Last year, 922 people in B.C. died of overdoses linked to the illicit drug.
The Liberal government has pledged $65 million over five years to fight the opioid epidemic, with $10 million in urgent support for B.C. On Friday, Prime Minister Justin Trudeau sat down with emergency responders, healthcare workers and families of victims to discuss the response.
But as fentanyl continues to be sold across Canada -- often disguised as other drugs -- Jansen’s mother says the Liberal government must make a bigger investment to quell the crisis.
“A $10 million federal contribution towards the opioid crisis in B.C. is far, far too low,” Michelle Jansen told CTV’s Power Play on Friday. “The amount that is being contributed now is far from enough and, in my opinion, I think it stems from the stigma of addiction.”
Government oversight need
The problem goes beyond money, Jansen says. She’s calling for more oversight into privately-run drug treatment facilities, like the one where her son died after he had a drug dealer drop off fentanyl at the facility.
An inquest was held into Jansen’s death in January, which determined that his death was accidental. The report found that the Sunshine Coast Health Centre was in compliance with Vancouver Coastal Health Authority regulations.
“There are no regulatory requirements for addiction centres in order to make sure that clients are receiving the medical treatment and the therapy and the supervision and the security to keep them safe. And that’s exactly why my son died.”
Jansen says she spent more than $200,000 on private treatment for her son’s addiction, and that the Sunshine Coast Health Centre was the 11th drug-treatment centre he visited.
With the anniversary of Brandon’s death next Tuesday, Michelle Jansen said she wants Canadians to understand just how easily young people are getting fentanyl -- oftentimes without knowing they’re taking the dangerous drug.
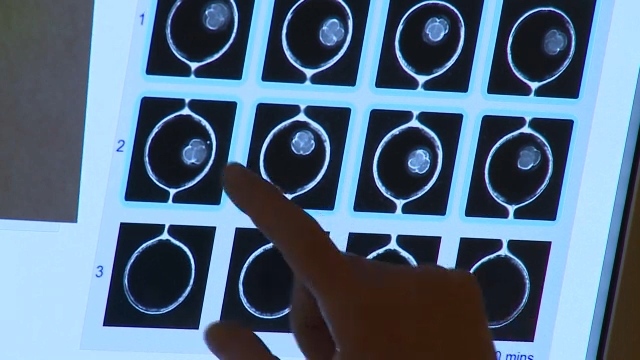
“He was recreationally taking drugs. He had no idea that he was using fentanyl. It was being sold out on the streets and being given at parties as prescription (oxycontin), which it was not,” she said. “The drug is so powerful that it takes a hold of your brain.”
Frontlines of opioid crisis
The crisis has put a major strain on Vancouver’s Downtown Eastside, where fentanyl use is rampant. Last December, six people in the neighbourhood died from fentanyl overdoses in an eight-hour span. The issue has prompted emergency workers, such as paramedics and police, to work overtime and request more help from the government.
Sarah Blyth co-founded a pop-up injection site alongside a team on volunteers to monitor drug users in the community and, when necessary, administer life-saving doses of naloxone.
About two people per day visited the Overdose Prevention Society when it opened last September, Blyth said. They now see about 400 people per day.
“It is definitely a national crisis,” Blyth told CTV News. “It’s unlike anything that I’ve ever seen … and it’s happening to our most vulnerable citizens.”
Blyth points to stigma as the reason that the problem has escalated so quickly. Those with mental and physical health issues are disproportionately affected, she says.
Ahead of Trudeau’s visit, Blyth said she hoped the prime minister would expressly recognize that fentanyl has reached a level of national crisis.
Trudeau’s Friday meeting with those affected by the fentanyl crisis was a positive one, according to a health care official at the table.
“He was definitely emotionally impacted by the stories and I think the sheer magnitude of this crisis and all the work that’s being done in British Columbia trying to manage it is certainly something he understands,” said Linda Lupini, executive president of B.C. Emergency Health Services.
Lupini said she was “encouraged” by the prime minister’s response and said Trudeau seemed particularly interested in boosting funding for safe injection sites to allow the facilities to operate for longer hours.
“I think we are finally getting some recognition that B.C. has been dealing with something really, really difficult that will move across the province. We’ve been leaders in trying to deal with it, and I think the federal government does understand that,” she said.
Speaking after the meeting, Trudeau said the country must join forces to “help our most vulnerable.”
“This is a crisis that seems, for most Canadians, to be very far away. Something that’s limited to certain tougher parts of town, to the West Coast, but we are seeing a spread of opioids across the country and we’re seeing it spread far and wide across socio-economic levels, across communities.”
Jansen said she’s glad the government is discussing long-term plans for curbing the crisis, but that a swifter response is needed.
“We don’t have the luxury of long-term plans. People are dying in high numbers every single day. I want the government to treat it like the emergency situation that it is.”