OTTAWA -- Health care providers across the country are starting a research project to monitor what they say will be the adverse effects of federal government cuts to health-care benefits for refugees.
As of this weekend, the government will no longer cover the cost of extended benefits such as medication and vision care for refugee claimants.
And for some claimants, the only access to health care they'll have at all is if they pose a danger to public health.
The Canadian Doctors for Refugee Care says the cuts could have deadly consequences as refugees arrive in Canada with medical problems often related to their living conditions abroad.
Meanwhile, denying access to medicines to treat diabetes or heart problems also puts refugees' health at risk, they say.
If the government doesn't want to pay attention to those risks, doctors will, the group said Wednesday.
The data from the refugee health outcome monitoring and evaluation system, or HOMES, will be used to show the Conservative government the consequences of a policy decision made with no public debate, they told a news conference.
"The government is hurting our patients," said Dr. Philip Berger, chief of family and community medicine at St. Michael's Hospital in Toronto. "We will not stop ever and we will not forget.
"The Conservative government, if they reverse the health cuts to refugees, could make Canada Day in 2012 a day of pride, a day to celebrate our historically best qualities of caring, fairness and just giving people a chance."
The government argues that people awaiting a decision on a refugee claim shouldn't be entitled to better health-care coverage than many Canadian citizens, nor should those whose refugee claims are ultimately denied.
"With this reform, we are also taking away an incentive from people who may be considering filing an unfounded refugee claim in Canada," Immigration Minister Jason Kenney said when he announced the changes in April.
"These reforms allow us to protect public health and safety, ensure that tax dollars are spent wisely and defend the integrity of our immigration system all at the same time."
In a statement, Kenney's department said the doctors are welcome to share their study's findings.
"We are always interested in looking at studies related to refugee health outcomes as long as methodology is sound and the results are evidence-based," the e-mailed statement said.
The changes to the benefits divide refugee claimants into two groups.
One includes those whose claims are rejected or who are from countries on a yet-undecided list of safe countries and the other takes in refugees who are settled by government or are from countries deemed unsafe.
The former group will receive health care only to prevent or treat a disease posing a risk to public health or a condition of public safety concern, while the latter will still have access to some basic care.
But neither will have the cost of dental or vision-care covered and medicine will only be paid for if it is to treat a public health risk.
In their statement, the department said the program is not responsible for access to and delivery or medicines.
"As any insurance plan, we provide coverage for certain services and products," the statement said.
"People can still access denied services and products via other means as do a number of low and modest-income working Canadian who do not have access to social assistance programs or employer insurance."
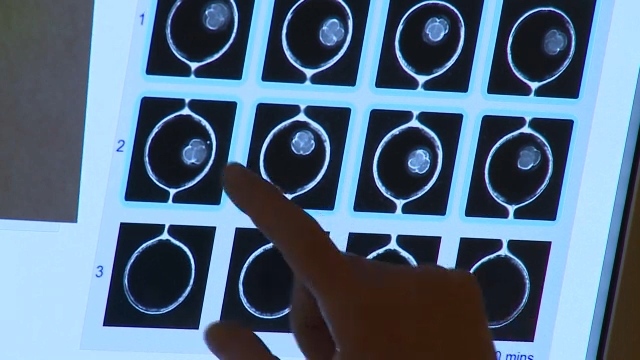
The definition of a public health risk will be determined using a list of diseases drawn up by the Public Health Agency of Canada.
That list currently includes chickenpox, tuberculosis, malaria and AIDS.
The government says the cuts will save $20 million a year for the next five years.
The doctors argue those costs will be downloaded to the provinces.
"Not paying for these medications are going to have these patients (leaving) the emergency department, going home and coming back," said Dr. Parisa Rezaiefar, a family doctor and emergency room physician at the Children Hospital's of Eastern Ontario.
"This is an off-loading of our health-care money from the federal budget to provincial health plans and we are going to all pay for that."
Doctors have been protesting the cuts for weeks and have been showing up at various events featuring federal ministers this week in order to challenge the policy decision.
Dr. Megan Williams, an Ottawa family physician, went to an event Wednesday with the federal health minister to voice her concerns.
She said she's already having uncomfortable conversations with some of her refugee patients, including a recent one with a patient who has diabetes.
The pharmacy would only give enough medication to last until the end of the month, Williams said.
"They came back to me and said: 'What am I going to do?'
"(This patient) will not the very next day die, necessarily, but they certainly will over the first week of July become very sick.
"They're probably going to end up in the emergency department and that is going to cost a lot of money and will have negative effects on the health system."