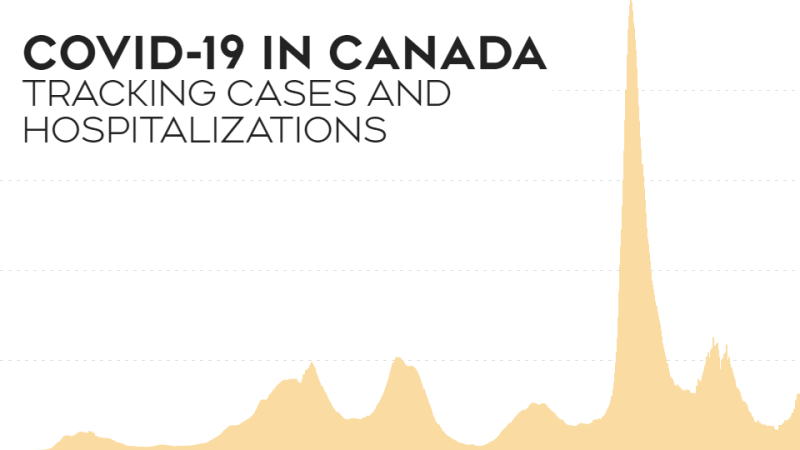
TORONTO -- Concerns over blood clots in patients who have received the AstraZeneca vaccine may further slow the vaccine rollout in Canada.
Provinces are reconsidering their rollout plans in light of new guidelines from NACI to avoid use of the AstraZeneca vaccine in people under the age of 55. NACI’s updated guidelines comes after 31 people in Germany developed blood clots after receiving the AstraZeneca vaccine, nine of them died.
In Germany, 2.7 million people have received the AstraZeneca vaccine, this puts the chance of getting a blood clot at about one in 100,000, as opposed to a one in a million chance,according to the World Health Organization (WHO). The European Medicines Agency shared similar data, with 25 people out of 20 million developing blood clots.
“The odds of dying in a car crash are one in 100, to put that in perspective,” Rodney Russell, professor of virology and immunology at Memorial University of Newfoundland, told CTVNews.ca in a phone interview on Tuesday.
“It still puts it in the same range as dying by getting hit by lightning, but it sounds a lot worse,” he said.
The general adult population has a one in 1,000 chance of developing a blood clot in a given year. This is 100 times more likely than the risk associated with the AstraZeneca vaccine.
While the rare cases of blood clots are concerning, Russell is also worried about what this may do for Canada’s vaccine rollout. Canada is set to receive 1.5 million doses of the vaccine by April 4.
“The key to getting back to normal is for everyone to get vaccinated,” he said.
He said that reports saying that people aren’t showing up to get their vaccines indicates that there’s already a high rate of hesitancy among Canadians.
Pfizer and Moderna vaccines came out of the gate with 95 per cent efficacy rates, a number that was much higher than anticipated, he said. When AstraZeneca released their data with a lower efficacy, people began to prefer one over the other.
He said it’s important that people understand that each vaccine will have the same end result: preparing the body to create an immune response to the SARS-CoV-2 spike protein.
“It's the protein at the end of the assembly line that gets seen by the immune system,” he said.
While the Pfizer and Moderna vaccines, which use mRNA technology, have a higher efficacy than the AstraZeneca vaccine, which uses viral vector technology, they all target the same protein.
The mRNA vaccines use molecules called mRNA to tell the body how to make the SARS-CoV-2 spike protein, while viral vector vaccines use genetically modified virus to deliver the instructions on making the spike protein, according to Health Canada. According to the CDC, viral vector vaccines have been studied since the 1970s and most recently two viral vector vaccines have been used in Ebola outbreaks. They say that mRNA vaccines are newer with Pfizer and Moderna being the first of their kind approved in Canada and the U.S..
Russell said that it’s unfortunate that the efficacy of the various vaccines have been focused on, leading to the public to label Pfizer and Moderna as good and AstraZeneca as bad. Real-world data has allowed AstraZeneca to increase the efficacy data from 62 per cent to 76 per cent.
The news of lower efficacy was followed by Health Canada’s approval of the vaccine for use in people under age 65, an age determined by a lack of data, not safety issues, he said.
“Don't forget, this is the vaccine that they mistakenly gave half doses in the phase three trial,” he added.
Since day one, AstraZeneca seems to be followed by bad news that Pfizer and Moderna have so far been able to avoid, and extra precautions are being taken to ensure the safety of the new vaccines.
“We're trying to show how careful we're being, but by doing that, then we're pausing every week for different reasons, at some point people start to think ‘well this is garbage and shouldn’t be put in our bodies because every week there's a new problem with it,’” he said.
If given the chance, Russell said he’d get the AstraZeneca vaccine today.
“I'd rather be vaccinated and watching for side effects than not know when I'm ever going to get a vaccine,” he said. “You still have 17 million people who've been vaccinated and not had any trouble.”
And there’s the trouble. Russell, like many Canadians, doesn’t know when he’ll be able to get the vaccine. He thinks it will be late summer, but in light of the latest data on AstraZeneca, it could be even later.
He said that a day or two of pauses may not cause a backlog, but if the pauses last for weeks it will cause delays and backlogs. Not to mention the potential for doses to expire and go to waste.
Canada’s rollout plan relies heavily on the use of AstraZeneca. The country has 20 million doses of the AstraZeneca vaccine on order.
“It has to increase hesitancy, which is going to slow down acquisition of herd immunity,” Russell said. “And it's vaccines that are going to get us there.”
The data surrounding AstraZeneca has cast doubt on the vaccine since the start. It’s efficacy wasn’t as high, the third phase of the trial used incorrect dosing, it wasn’t approved for use in those over age 65, and then it was. For the general public, this may be a cause for doubt in the approval process, but it shouldn’t be,said CTV News medical specialist, Dr. Marla Shapiro.
“When I look to the immediate response and how nimble and flexible we are as data evolves, it really does tell me that we should have confidence in our advisory bodies who are monitoring and really have a very high bar of safety here and really want to make sure that we're doing no harm,” she told CTV News Channel on Tuesday.
Anything that slows down the ability to vaccinate will result in a slower return to so-called normal life in Canada, said Russell.
It doesn’t help that different provinces are taking different approaches, leaving Canadians unsure of what to do. People will wonder why their province didn’t pause it, or wonder what their province knows that others don’t, he added.
A single voice from the government about why there is changing information could help ease some concerns.
“I do think we need a much better communication strategy, we need a single, solid voice explaining to the Canadian population where the information is coming from, why we're responding the way we do. We need to be completely transparent,” said Shapiro.