One in 18 patients suffered potentially preventable injuries after being admitted to Canadian hospitals, according to a new study.
Data collected by the Canadian Institute for Health Information (CIHI) and the Canadian Patient Safety Institute (CPSI) shows patients experienced unintended trauma that required treatment and extended their stays in 138,000 hospital visits between 2014-2015. Roughly 2.5 million patients were admitted over the course of the study, which did not include hospitals in Quebec.
The analysis, based on a new measure developed by CIHI and CPSI, looked at 31 types of injuries. They ranged from preventable actions that should never occur, such as cases where surgical instruments were left inside a patient’s body, to less preventable risks like contracting pneumonia.
Health-care and medication-related trauma such as bed sores and the side effects of receiving the wrong medication accounted for 37 per cent of the documented incidents. Infections made up an additional 37 per cent, followed by procedure-related trauma like bleeding after surgery (23 per cent), and patient accidents (3 per cent). Multiple forms of patient harm were involved in one out of every five cases.
The findings have been compiled in a new risk prevention resource for medical professionals aimed at improving patient safety.
“While most patients experience safe care in Canada, we must continually strive to do better,” Health Minister Jane Philpott said in a news release Wednesday.
Tracy Johnson, director of health system analysis at CIHI, said the majority of patients are safely cared for in Canadian hospitals. But it’s important to recognize that mistakes and accidents do happen, andhospitals should focus on prevention and education, she said.
“It’s important to understand that (patient harm) is preventable … because we can do something about it,” Johnson told CTV News Channel on Wednesday.
The CIHI/CPSI report found that one in eight hospitalizations involving a “harmful event” ended with the patient’s death. But a direct link between the harm and the death cannot be determined by looking at the administrative data collected in the study, the report notes.
“Death might be due to the harmful event, or it could be that the patient was at higher risk of dying because he or she had more complex conditions,” the report says.
‘It happened right in front of me’
Carole Jukosky said a communications breakdown between on-call physicians allowed her 72-year-old father, Herbert Strasser,to develop a series of infections that caused his death in September 2011 after a six-week stay in hospital.
“He would have been alive if these errors had not occurred,” she told CTV News. “I was there as often as I could be. It happened right in front of me. I didn’t recognize it until it was too late.”
Jukosky, herself a nurse administrator at a long-term care facility, said her father received an “inaccurate” urinary tract infection diagnosis following surgery for a stroke that did not account for a serious secondary infection site. He eventually contracted C difficile from antibiotic use, forcing him to battle three infections at once.
“My dad said to me they are going to kill me in here, and I sort of laughed it off,” said Jukosky, who once stopped her father from gulping down a cup of unidentifiable pills after losing confidence in his caregivers.
Jukosky said her father was shuffled between a number of Ontario health care centres after leaving hospital prematurely. He developed complications in rehab, but the hospital said he did not need to be readmitted.
“Everybody saw what happened. Everybody documented what was going on symptomatically. Nobody did anything about it,” she said.
‘A huge step in the right direction’
Saskatchewan nurse Donna Davis has been sharing the story of her tragic loss in an effort to raise awareness about patient safety across Canada.
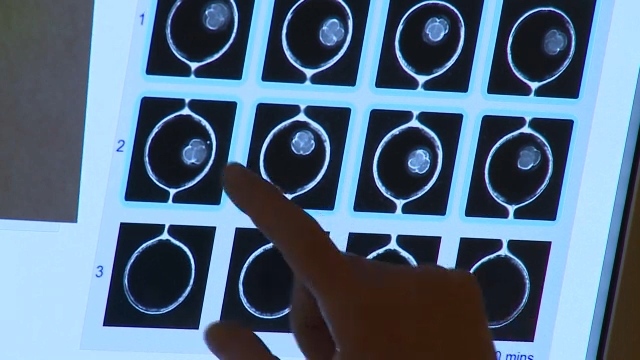
Davis’s 19-year-old son Vance died in 2002 after he was admitted to hospital with a head injury sustained in a car accident. Davis said she was very concerned about Vance’s condition throughout his hospital stay, but doctors and staff dismissed his injury as minor.
“My concerns fell on deaf ears,” Davis told CTV News Channel Wednesday.
She also said that there was a lack of communication among hospital staff.
Davis, who is now the co-chair of Patients for Patient Safety Canada, a CPSI program, said she wishes she had “the courage to speak up” as her son’s condition worsened.
Back then, “people didn’t talk about harm -- it was swept under the rug,” Davis said.
“It was a very hard thing for people in health care to accept that the care that was intended to heal people was actually harming them. (Health-care) providers don’t go to work to harm people and it’s very devastating when they have to face the fact that the care they did give caused harm.”
Davis said the latest report on patient harm is “a huge step in the right direction” toward educating health-care workers, patients and their families about the risks associated with hospital stays.
She said anyone providing care has to be vigilant, aware of best practices and the fact that every patient is different.
Both Davis and Johnson encourage patients to ask plenty of questions and be “active partners” in their medical treatments.
“Hospitals, as well as physicians, welcome patients being involved in their care,” Johnson said.
The CPSI has safety tips, resources and a checklist on its website for both patients and health-care providers.
With a report from CTV’s medical specialist Avis Favaro and producer Elizabeth St. Philip

Source: Canadian Institute for Health Information, Canadian Patient Safety Institute