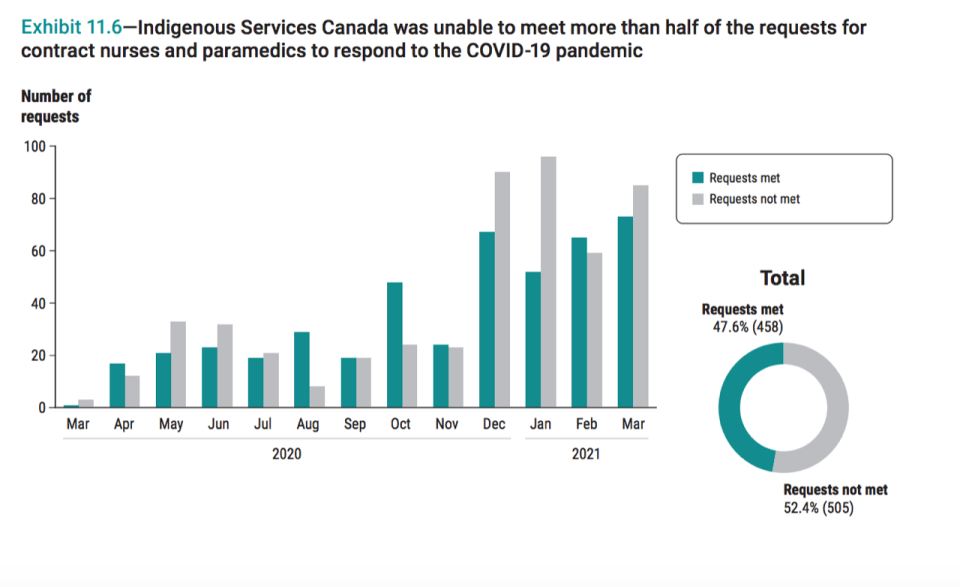
OTTAWA -- Indigenous Services Canada failed to uphold more than half of the requests it received for additional nurses and paramedics amid the pandemic, federal auditor general Karen Hogan says.
In an audit released Wednesday, Hogan said while the department made attempts to boost access to health-care workers in remote and rural communities, of the 963 requests for additional medial staff, 505 weren’t met.
“Like everywhere else across the country, the demand for nurses was growing exponentially and there was quite a shortage. But here I would point to really a long standing issue that exists with having access to proper health care in Indigenous communities,” said Hogan in a subsequent press conference.
"This longstanding issue is one that needs to be addressed."
The department also didn’t have “complete and accurate data” on its stockpile of personal protective equipment, nor did it initially have sufficient amounts of necessary medical supplies, but it nevertheless “adapted quickly” with efforts starting in April 2020.
“The department was able to secure additional PPE and quickly provide it to Indigenous communities and organizations when provinces and territories were unable to do so,” reads a press release.
The audit focused on whether Indigenous Services Canada “provided sufficient personal protective equipment, nurses, and paramedics to Indigenous communities and organizations in a coordinated and timely manner in order to protect Indigenous peoples against COVID-19.”
Indigenous Services Minister Marc Miller welcomed the findings of the report while speaking to reporters later in the day, commending the work of his team in uncertain times but also acknowledging more can be done to prepare for the future.
“This isn’t about being perfect, it's about realizing the cards that had been dealt to us and to work with providers in record time trying to outpace a virus that moves faster than government, and that’s what we did,” he said.
“We do know we can always do more and the real success story of this pandemic is that we are doing all of this hand in hand with First Nations, Metis and Inuit leaders.”
Earlier in the day he said the department is currently aware of 9,195 positive COVID-19 cases in Indigenous communities. In total, more than 28,000 people have recovered and 333 have died. He also said, as of this week, 75 per cent of Indigenous adults had received at least one dose of a COVID-19 vaccine.
On staffing requirements, Hogan stated that Indigenous Services Canada streamlined the hiring process for nurses to work in remote or isolated First Nations communities, created new positions for nurses and paramedics and expanded their jurisdiction, but ultimately couldn’t fulfill all needs.
“Indigenous Services Canada should work with the 51 remote or isolated First Nations communities to consider other approaches to address the ongoing shortage of nurses in these communities and to review the nursing and paramedic support provided to all Indigenous communities to identify best practices,” Hogan recommended.
The auditor general noted that in 2014, Indigenous Services Canada developed its own PPE procurement strategy in case of a communicable disease outbreak but “found that the department did not follow this approach and therefore did not have sufficient amounts of PPE items at the beginning of the pandemic.”
As time went on, the department bolstered its stockpile, which included an agreement of two per cent of the bulk supply secured by the Public Health Agency of Canada, and ultimately responded to 1,622 requests for PPE “in a timely manner” within 10 days of when the request was initially made.
Due to troubles with the department’s PPE tracking system, the department actually logged more supply than it needed at times.
“On one occasion, the department took action to temporarily stop shipments of hand sanitizer because of safety concerns related to its storage,” the audit reads.
Hogan acknowledged that some of the tracking issues are reflective of the jurisdictional complexities at play during a health crisis like COVID-19 and the involvement of all levels of government.
“There’s a need for information sharing agreements to be ironed out and while those things hadn’t happened prior to this pandemic we did see that the provinces and territories and the federal government collaborated together in order to address needs,” she said.