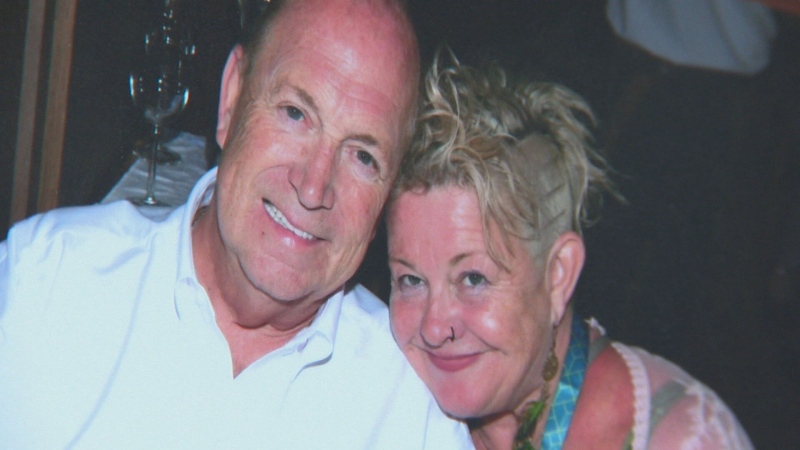
Elizabeth Ostrander spent two years on an organ transplant wait list, worrying about her oxygen levels any time she left home and wondering if she'd ever get the lungs she needed.
The Niagara, Ont., resident, who was diagnosed with chronic obstructive pulmonary disease (COPD) in 2016, underwent a successful double-lung transplant in November. But she came close to scheduling her surgery a couple of times before that - only to discover the lungs she was set to receive weren't a good match for her B-positive blood.
Ostrander's wait was much longer than most lung transplant recipients, who can get new organs within a few months depending on where they're located in the country, with patients at transplant centres in big cities often having shorter wait times.
While she's doing well now, Ostrander still wishes her surgery came sooner.
“I was on oxygen for six years - always worried about running out, getting tangled up in the tubing or having them fall off at night,” said the 57-year-old, who had her surgery at the University Health Network's Ajmera Transplant Centre in Toronto.
A new study from Canadian researchers is providing hope for potential transplant recipients, especially those like Ostrander who have rare blood types or other physical factors that increase their time on waitlists.
The proof-of-concept study, published Wednesday in Science Translational Medicine, suggests organ blood types can be converted to universal O, which authors say could expand the pool of universal donors, improve fairness in organ allocation and decrease mortality for patients awaiting life-saving surgeries.
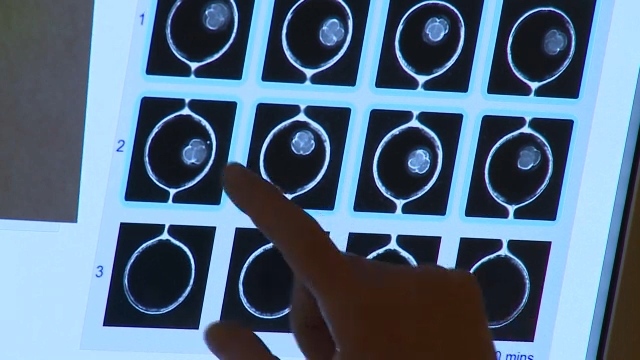
Researchers at UHN treated eight lungs that weren't suitable for transplant with a pair of enzymes that converted the organs' blood type from A to O without causing any lung toxicity. The enzymes removed more than 97 per cent of blood type A antigens within four hours.
Antigens in blood can trigger an immune response to foreign substances in the body and reject organs unless they match the recipients' blood type or come from universal type O donors.
Dr. Marcelo Cypel, a thoracic surgeon at UHN and one of the study's authors, said the enzyme process was developed by University of British Columbia biochemist Dr. Stephen Withers and his team in 2018 to convert red blood cells for transfusions.
Cypel's team tested the enzymes in blood and then in a human aorta. Once they saw success, they moved onto a whole organ.
Three of the converted lungs were tested for rejection by introducing blood with A and AB-antigens, and Cypel said results were favourable.
“We knew this was very efficient based on Dr. Withers' previous work in blood cells (but) it's much easier to take a bag of blood and put the enzyme in and ... distribute it quickly,” Cypel said. “To reach all the other facets of the organ tissue, we didn't know if we'd get to that point.
“So I was pleasantly surprised we were able to have such an efficient depletion of these antigens. And when we reintroduced blood into the system ... we could clearly see it didn't react adversely with the organ, which was very different for the organs that were not treated with the enzyme.”
The research focused on lungs but Cypel said it will likely work on other organs. The team is expanding its research to kidneys next and aims to progress to human clinical trials within 12 to 18 months.
Proof-of-concept studies help determine whether something is feasible before further analysis can take place. Cypel said the study is a first step that offers promise for those waiting for specific blood-type organs.
Currently, people with A or B blood can receive O type organs, but those with O blood can only receive from other O donors. Cypel said that means that sometimes, those in most need of transplants are skipped for patients on the waitlist who may be less sick but match the organ's blood type.
Patients who are type O wait on average twice as long to receive a lung transplant compared to patients who are type A, the researchers say. They are also 20 per cent more likely to die while waiting for a transplant.
Other blood types, including Ostrander's B-positive, can see extended wait times because B donors are also rare, said Cypel, who was Ostrander's doctor.
The Canadian Blood Services website says O-positive is the most common blood type in Canada at 39 per cent, while A-positives make up 36 per cent of the population. Less than eight per cent of Canadians are B-positive and 1.4 per cent are B-negative, the rarest blood type in the country.
Cypel added that Ostrander also had to wait for a lung size that matched her small frame, which further diluted her options from donors.
“When you start to (include) other factors, finding a small B donor takes a long time,” he said. “So B patients will benefit from this too because ... an A donor which is converted to an O donor can be used by any A, B or O.”
Ostrander said potentially changing an organ's blood type to make it suitable for any patient would help people avoid waiting years for a transplant.
“It would have made so much difference in my life,” she said. “I would have had more freedom. I'd be able to go out with my family more often, go camping - things you used to do that you could no longer do.”
This report by The Canadian Press was first published Feb. 16, 2022.