TORONTO -- Sepsis, the catastrophic condition that took the life of actress Patty Duke this week, is among the most difficult to treat and often ends in death. But a group of Canadian researchers hopes to change that grim outcome with an innovative therapy using injections of specialized stem cells.
In an experimental trial, researchers at the Ottawa Hospital are testing mesenchymal stem cells from a healthy donor in patients admitted with sepsis, a runaway infection that invades the body, leading to multiple organ failure and ultimately to septic shock. The condition is fatal in 20 to 40 per cent of cases.
Sepsis can arise from infection from bacterium, viruses or fungus -- even in some cases one that starts with a cut in the skin, said Dr. Lauralyn McIntyre, an intensivist who is leading the clinical trial.
The condition affects an estimated 40,000 to 50,000 Canadians each year and is most common in those with compromised immune systems, such as the very young, the elderly and those with chronic diseases like HIV, cancer or diabetes.
Duke developed sepsis and then progressed to septic shock after her intestine ruptured. But the condition can arise from any number of infections, including pneumonia and those affecting the kidneys, urinary tract or bloodstream.
"(The latter) can occur just from a bug entering your skin and going into your bloodstream and then just wreaking havoc," McIntyre said.
However, it's not so much the microbe behind the infection that leads to sepsis -- it's the body's response to that infection. Sepsis occurs when the immune system gets hyperactivated, causing rampant inflammation in many parts of the body, including the brain, vital organs and the cardiovascular system.
"Even your bone marrow and your blood begins to fail," said McIntyre, explaining that as the organs and other internal systems begin shutting down, blood pressure plummets and the person goes into septic shock.
"It can be a devastating problem."
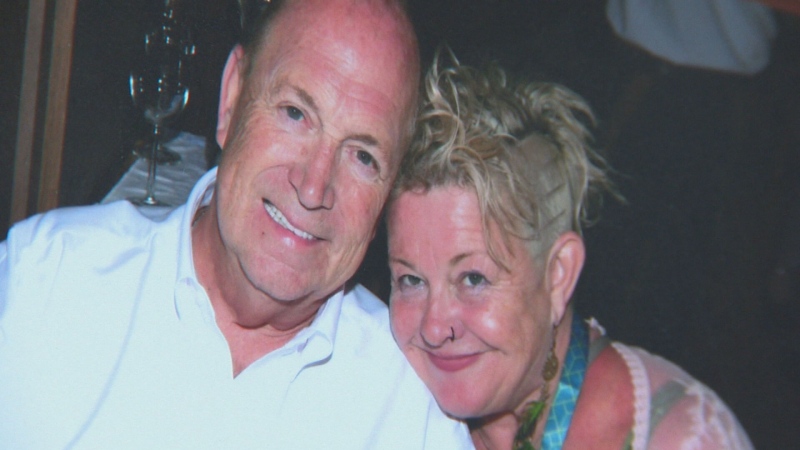
Charles Bernique of Hawkesbury, Ont., 73, developed sepsis last June after his esophagus ruptured and he developed an infection, possibly as a result of severe food poisoning.
At the Ottawa Hospital, surgeons repaired his esophagus, then kept him in an induced coma for four days while the ICU team pumped him full of antibiotics to fight the infection, supported his lungs with mechanical ventilation and his failing kidneys with dialysis.
With Bernique close to death, the hospital approached his wife Maureen with a proposal: would she be willing to enrol her husband in a trial for an experimental therapy using stem cells, in the hope the treatment might help him recover?
With her consent, her husband was injected with 30 million mesenchymal stem cells, which researchers believe may tamp down severe inflammation, based on animal studies that showed they can overcome sepsis and significantly reduce mortality.
After three months in the ICU and another month or so recovering at home, Bernique was restored to health and was able to return to work at an egg-production facility near his hometown.
"This to me is a miracle that I'm where I am now," Bernique said Thursday from Ottawa. "I'm back working and I'm doing the things I could do before."
Researchers can't yet say if it was the stem cells that saved his life -- their Phase 1 study of nine patients is designed to determine if the treatment is safe -- but co-investigator Dr. Duncan Stewart, head of the Ottawa Hospital Research Institute, said results so far look promising.
For the last decade, Stewart has led a team investigating the healing potential of stem cells in lab rodents with induced sepsis, as a prelude to testing in humans.
"And we were quite surprised actually in ... the degree of benefit we got," he said, noting that the mesenchymal stem cells appeared to not only reduce inflammation, but also to help clear the infectious pathogen from the animals' bodies.
In the body, mesenchymal stem cells can develop into various tissues of the lymphatic and circulatory systems, and into connective tissues such as bone and cartilage.
Scientists aren't sure how injections of these cells work, although they appear to travel to the sites of injury and to have a modulating effect on an overactive immune system. The cells, which are derived from a donor's bone marrow but don't require a recipient to take antirejection drugs, are eventually cleared naturally from the body.
"We know they don't permanently engraft into the host," Stewart said. "They're there for days or weeks and then they're removed, which is just what you want in an acute disease like sepsis."
Researchers have been seeking an effective treatment for sepsis and septic shock for decades; a number of drugs have been tested in clinical trials, but they have not proven successful.
Stewart hopes that won't be the case with the stem-cell therapy, but that won't be known until the team determines its safety and moves onto a Phase 2 study that would enrol many more patients with severe sepsis to determine whether the treatment works.
So far, patients in this trial have shown no adverse reaction to the stem cells, and there have been "hints or glimpses of efficacy," he said.
"What I can tell you is things have gone very well so far, so it looks like this has been very safe and the results have certainly been encouraging enough that we've got a lot of enthusiasm for moving forward."