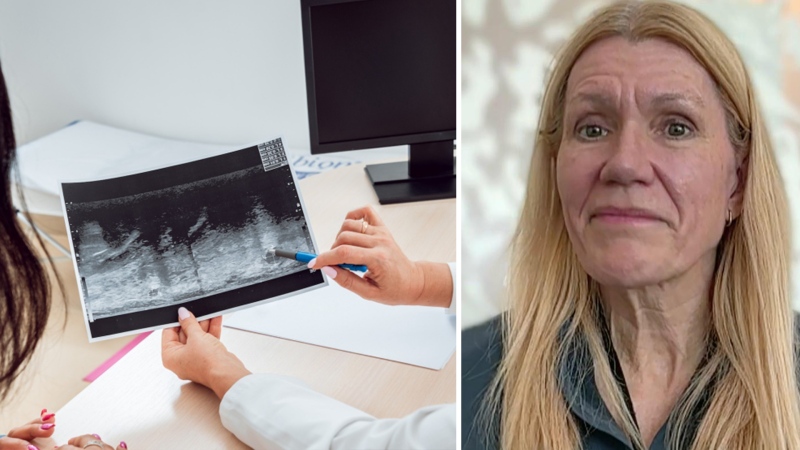
New guidelines informing the care of perimenopausal and post-menopausal woman in Canada have been released, backed by new data to help physicians know when to prescribe menopausal hormone therapy — and when it might not be worth potential risks.
Post-menopause, women are at a higher risk for a number of health conditions, including cardiovascular disease. Doctors want to ensure any treatment a patient undergoes due to menopause doesn’t increase those risks even further.
The updated guidelines state that menopausal hormone therapy is the most effective treatment for the relief of menopause symptoms.
Researchers found that long-term data showed that short-term menopausal hormone therapy did not come with increased cardiovascular risk when appropriately prescribed to women who were not at a high risk for heart problems.
However, if women initiate menopausal hormone therapy 10 or more years after they hit menopause, they may be at an increased risk for adverse cardiac events.
Dr. Beth Abramson, a cardiologist, professor at the University of Toronto and one of the authors of the new guidelines, told CTVNews.ca in a phone interview that each individual patient has individual risks and circumstances to weigh, but that these guidelines help doctors have the tools to understand those.
“There have been several studies and analyses that have come out in the last few years to inform and appropriately give health-care providers the information to have a conversation with their female patients,” she said.
“The women who are under 60 years of age who've had menopausal hormone therapy initiated shortly after their last menstrual period, there seems to be no increased risk for cardiovascular disease. And we have seen in general, there's low risk for adverse events, including stroke, in the next few years.”
WHAT IS MENOPAUSAL HORMONE THERAPY?
Menopause marks the end of the stage in a woman’s life in which she has menstrual periods and can become pregnant, usually experienced in midlife.
During this transition, the body’s production of estrogen and progesterone varies heavily, and after menopause, a woman’s body will be producing far less estrogen. Menopause can sometimes be triggered by the removal of the ovaries or certain ovarian diseases or cancers.
While some women experience few symptoms during the years of menopausal transition or perimenopause, others can experience a range of symptoms, including hot flashes, vaginal dryness, sleep problems, trouble controlling one’s bladder, mood changes and chills, among others.
“If a woman has those symptoms, and they’re severe, treatment can be indicated for someone's quality of life,” Abramson said.
According to Mount Sinai Hospital, around 80 per cent of women have some menopausal symptoms, and 20 per cent of these women experience severe ones.
The most effective treatment for those with severe symptoms is menopausal hormone therapy (MHT), according to the guidelines.
It works by giving menopausal women estrogen, usually combined with progesterone, that the body is no longer producing.
“It's giving back the estrogen that is depleted or falls when a woman's body changes after midlife,” Abramson said.
But there are considerations to make when prescribing MHT.
“Estrogen is a hormone and a hormone by definition has multiple effects on the body,” Abramson said. “And the issue with estrogen is that there is a consistently small, but important, increased risk of blood clots in the legs and the lungs. We call it venous thromboembolism. That has to be weighed against the risk of benefit to that individual patient.
“And so our guidelines have looked at the evidence before us. I think we're much more informed than we were a decade or so ago.”
BREAKING DOWN THE GUIDELINES
The new guidelines, written in collaboration with the Society of Obstetricians and Gynecologists of Canada and presented this weekend at the Canadian Cardiovascular Congress in Ottawa, are aimed at physicians, family doctors, nurses, pharmacists and other health professionals.
Researchers consulted relevant studies published on PubMed, MEDLINE and the Cochrane Library between 2002 and 2020 to update the guidelines.
They found that short-term menopausal hormone therapy treatment did not correlate with an increased cardiovascular risk in appropriately selected patients.
Abramson explained that short-term means that MHT is not taken for a prolonged period or indefinitely.
“So we're not talking about 10 years of therapy, for example,” she said. “Most of the data that suggests safety looks at women who have had roughly five years of therapy, and then they stopped.”
The data they looked at continued to track patients for years after they ceased MHT, up to 18 years after in some studies, in order to measure if there were long-term risks.
These studies showed that “there is not an increased risk of heart attack or stroke in these women,” Abramson said.
The guidelines suggest that doctors who have decided MHT is suitable for their patient should prescribe the lowest dose of estrogen that still addresses an individual’s symptoms, in order to minimize the risk of stroke and blood clots.
Researchers also found that providing MHT to women who had hit menopause early, and continuing to provide that therapy up until the average age of menopause, seemed to decrease the risk of adverse cardiovascular outcomes.
The average age of menopause is around 51.
Previous research has found that women who start experiencing menopause prematurely may be at an increased risk of coronary heart disease.
“We certainly know that older women who are over 60, who've been out 10 years post-menopause, have a higher risk of (blood) clotting, and we don’t recommend menopausal hormone therapy in general (for them),” Abramson said.
She added that it’s important to note that MHT is intended for relief of symptoms associated with menopause, not for the purpose of preventing cardiovascular disease, and isn’t recommended for that.
Abramson noted that more research still needs to be done to assess the delivery method of MHT.
“There's lack of high quality data, looking at what types of estrogen that we need to give our female patients, whether it's by mouth or in a patch over the skin, for women who are at average cardiovascular risk, and I think there's room for ongoing research to evaluate that,” she said.
While the new guidelines themselves don’t differ too greatly from the older 2014 guidelines, they have much more data to back them up, Abramson said, particularly in assessing individual risk and benefit.
Many women will never need MHT, but the option is there for those who do. This continued research helps to ensure that doctors are able to help patients make those decisions, experts say.
“I think a woman who's having symptoms should talk to her doctor, because we have data to have an intelligent and informed discussion to make sure that that woman is aware of the risk versus benefit,” Abramson said.
“If we don't discuss, we can't treat.”