The World Health Organization (WHO) has updated its guidelines for the treatment of COVID-19 patients, including categories of hospitalization risk to help doctors tailor treatment, and recommendations surrounding a new antiviral designed specifically to tackle the disease.
The new guidelines released Thursday evening include detailed recommendations for different drugs based on whether patients with non-severe cases of COVID-19 have a low, moderate or high risk for hospitalization.
The guidelines also adjust hospitalization risk thresholds, which could also make it easier for people with non-severe COVID-19 to get access to medication to treat their infection.
- COVID-19 Brief newsletter: Sign up for fresh insights and analysis on the pandemic
- Top coronavirus headlines, all in one place
The threshold for considering whether a drug is worth prescribing to a patient with a mild case has been lowered from a six per cent reduction in hospitalization to a 1.5 per cent reduction.
The guidelines also go over drugs the WHO does not recommend, including new warnings for ivermectin.
This is the 14th update to the guidelines, which have been evolving over the past three and a half years as the clinical understanding of the virus evolves, along with the virus itself.
RETHINKING ‘IMPORTANT REDUCTION’ IN HOSPITALIZATION RISK
One of the new updates is the threshold for how effective treatment needs to be at reducing hospitalization risk in order to be considered for patients with non-severe COVID-19.
The guideline development group initially inferred that a drug would need to pass a threshold of at least a guaranteed six per cent reduction in the risk of hospitalization in order to even be considered to be prescribed to someone with a non-severe case of COVID-19. This means if a patient inquired about a treatment they had heard of, and it only guaranteed a five per cent reduction in hospitalization risk, doctors wouldn’t have prescribed it.
Under the newguidelines, WHO has decided that if a drug achieves at least a 1.5 per cent absolute reduction in the risk of hospitalization, this can still be viewed as an “important reduction” for patients with non-severe COVID-19, and can be considered for treatment.
This change is due to “increased availability of drugs and higher confidence in their safety profiles,” the guidelines say.
This doesn’t mean that every patient with non-severe COVID-19 will receive treatment that passes this newly lowered threshold, just that treatment no longer has as high a bar to clear in order to be considered by doctors.
SPLITTING NON-SEVERE COVID-19 PATIENTS UP BY HOSPITALIZATION RISK
This reassessment of the treatment benefit threshold goes hand in hand with a change to how hospitalization risk is defined.
If you have a severe case of COVID-19, hospitalization is probably a sure thing. But those with non-severe cases may still end up in hospital, depending on their risk factors.
While previous guidelines only identified high and low risk, the updated guidelines now add a moderate risk category. This is intended to help doctors focus treatment where it will have the greatest impact in keeping patients out of the hospital.
The majority of patients with non-severe COVID-19 are low risk, meaning their chance of hospitalization is 0.5 per cent.
Patients with non-severe COVID-19 are considered to be at a moderate risk (three per cent) of hospitalization if they fulfill one or more of these requirements: they are over 65 years old, have obesity, have diabetes and/or chronic cardiopulmonary disease, chronic kidney or liver disease, an active cancer, those with disabilities and those with comorbidities that come with chronic disease.
Patients with non-severe COVID-19 are considered to be at a high risk of hospitalization (six per cent) if they have diagnosed immunodeficiency syndromes, or are receiving immunosuppressants due to organ transplant or an autoimmune illness.
WHO’s definition of severe COVID-19 includes those with signs of pneumonia, severe respiratory distress, and/or oxygen saturation in the blood below 90 per cent, while critical cases include situations where a patient requires life-saving measures due to issues such as septic shock or acute respiratory distress syndrome.
UPDATED TREATMENT GUIDELINES FOR NON-SEVERE COVID-19
The guidelines surrounding treatment for critical cases of COVID-19 did not require an update in this new edition, but many drugs received updated recommendations for their use with non-severe cases of COVID-19.
Nirmatrelvir/ritonavir (Paxlovid)
Nirmatrelvir is a protease inhibitor medication that prevents the viral replication of SARS-CoV-2, the virus that causes COVID-19. It is administered to COVID-19 patients in conjunction with ritonavir, an HIV protease inhibitor that works to boost nirmatrelvir’s effects.
“The (guideline development group) concluded that nirmatrelvir/ritonavir represents a superior choice to the other drugs when available and in patients in whom drug interaction is not an issue,” the report stated, adding that it was found to be more effective than molnupiravir, an antiviral drug.
This is the only drug that is strongly recommended for use with patients with non-severe COVID-19 and a high risk of hospitalization.
The benefits are believed to be largely negligible for those with a low risk of hospitalization.
- Patients with high risk of hospitalization: nirmatrelvir/ritonavir use strongly recommended
- Patients with moderate risk of hospitalization: nirmatrelvir/ritonavir use conditionally recommended
- Patients with low risk of hospitalization: nirmatrelvir/ritonavir use conditionally recommended against
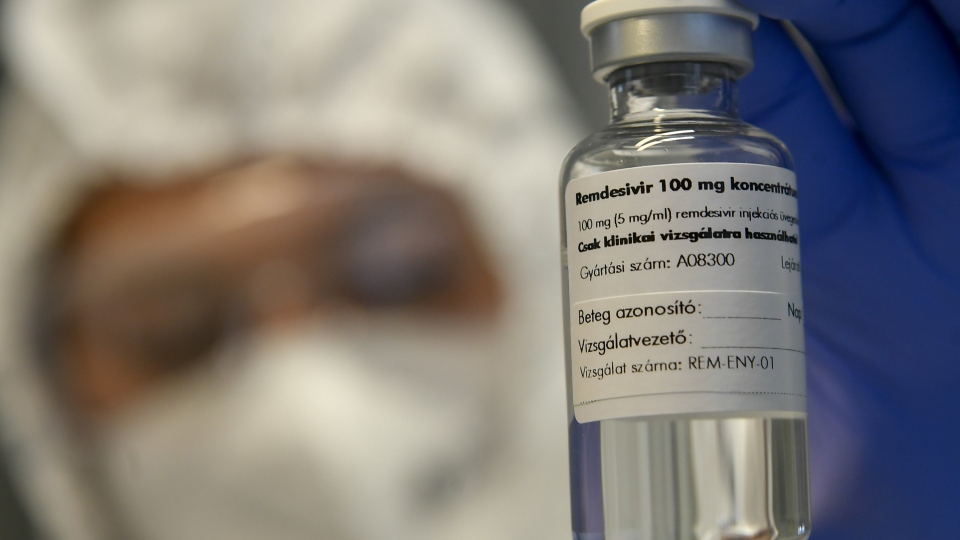
Remdesivir
An antiviral medication developed initially to treat hepatitis C, remdesivir has been the subject of numerous studies throughout the pandemic, with many pinning their hopes on it as a treatment. Early in the pandemic, its use was conditionally recommended against because studies didn’t show a statistically significant impact on patients.
This changed in 2022, when WHO conditionally recommended remdesivir specifically for non-severe COVID-19 patients at high risk for hospitalization.
In this update, WHO adds recommendations for the moderate and low groups.
- Patients with high risk of hospitalization: remdesivir use conditionally recommended
- Patients with moderate risk of hospitalization: remdesivir use conditionally recommended against
- Patients with low risk of hospitalization: remdesivir use strongly recommended against
Using remdesivir among low risk patients could “exacerbate health inequities by using significant resources for a negligible benefit,” the report stated, adding that it does not result in important reductions in hospital admission and has “little or no impact” on mortality.
Molnupiravir
An antiviral similar to remdesivir, molnupiravir may be an option for those who cannot tolerate other medications. However, WHO notes there is “residual uncertainty” regarding potential long-term harms as a result of its use, including the worry that it could contribute to the emergence of new COVID-19 variants.
- Patients with high risk of hospitalization: molnupiravir use conditionally recommended
- Patients with moderate risk of hospitalization: molnupiravir use conditionally recommended against
- Patients with low risk of hospitalization: molnupiravir use strongly recommended against
Other drugs
The use of several other drugs for patients with non-severe COVID-19 are covered in the guidelines, but did not require updates in this new edition. These include systemic corticosteroids (conditionally recommended against for any patient with non-severe COVID-19), fluvoxamine (conditionally recommended against except in the context of a clinical trial), sotrovimab (strongly recommended against for any patient with non-severe COVID-19) and colchicine (strongly recommended against for any patient with non-severe COVID-19).

UPDATED WARNINGS FOR USE OF IVERMECTIN AND A NEW ANTIVIRAL
VV116
When COVID-19 emerged in late 2019 and quickly spread across the globe in 2020, researchers immediately began to investigate which existing drugs could be repurposed to treat the virus. But researchers in China also began to develop a therapeutic aimed specifically at tackling COVID-19, which they presented preliminary research for in 2021.
Because VV116 was created to tackle COVID-19 specifically, research assessing its effectiveness is still new.
It is an oral antiviral drug which induces RNA chain termination to interfere with the spread of the virus. While WHO notes that it “does not seem to be associated with increased adverse effects,” there still isn’t enough data to recommend it at this stage, according to the agency.
Only one randomised control trial has formally assessed its effectiveness by comparing it with Paxlovid. Although the trial found that VV116 was noninferior compared to Paxlovid, no deaths were recorded in the entire trial, making it difficult to assess if the medication itself had any impact in preventing mortality, WHO stated. There was also no placebo control group in the trial.
The updated guidelines reflect that WHO strongly recommends against VV116 being used for COVID-19 patients regardless of how serious their illness is, except in the context of a clinical trial.
Ivermectin
Despite widespread use of ivermectin, a medication approved for use in humans to treat parasitic infections such as river blindness, it is still not recommended for use with COVID-19 patients in clinical settings, the WHO guidelines state.
But WHO is now also strongly warning against its use for those with non-severe COVID-19, even in research settings.
New research that has emerged since 2021 has reduced the uncertainty surrounding whether or not it is worth continuing randomised controlled trials assessing ivermectin’s usage for those with non-severe COVID-19, WHO states.
This data shows a “very low likelihood of benefit,” both due to research that has tested and also due to the “lack of biological basis for any effect of ivermectin on the virus.” Essentially, it was always scientifically unlikely that it would have an effect, and it hasn’t been shown to have one.
Ivermectin is conditionally recommended against in research settings for severe cases of COVID-19 as well.
“Use of ivermectin risks diverting attention and resources away from care likely to provide a benefit such as nirmatrelvir/ritonavir, remdesivir, and molnupiravir as well as supportive care interventions,” WHO states, adding that it risks causing drug shortages for those suffering from issues ivermectin is actually designed to tackle.
Drugs such as hydroxychloroquine, lopinavir-ritonavir, casirivimab and imdevimab are strongly recommended to not be used with any COVID-19 patients, according to WHO.