A growing number of older adults are living with human immunodeficiency virus (HIV) in Canada. But according to a Toronto-based charity, health-care systems currently in place are not prepared to care for the rising number of aging Canadians who are HIV-positive.
Toronto-based HIV/AIDS advocacy charity, Realize, says long-term care homes and health-care facilities across Canada are not equipped to treat older patients with HIV, who are more likely to experience chronic illness.
"They tend to be more likely to develop cardiovascular disease, diabetes, and other chronic illnesses that they have to manage on top of their HIV,” Kate Murzin, national program manager for Realize, said to CTVNews.ca in a phone interview Wednesday. "They're experiencing the overlap between HIV and aging now, and it's causing a lot of complexity in both their health, physical health, but also in terms of other social factors, for example, financial security in older adulthood.”
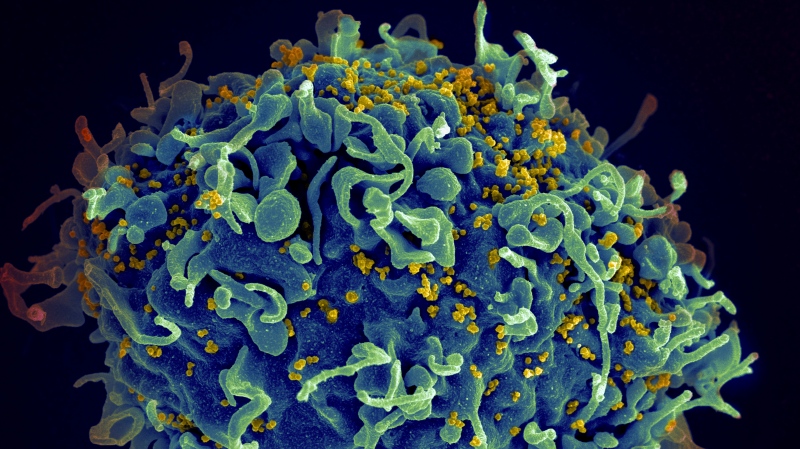
HIV is a sexually transmitted bloodborne pathogen. The World Health Organization (WHO) says HIV is an infection that attacks the body's immune system, specifically the white blood cells. If the virus succeeds in destroying these cells, a person's immune system is weakened. This allows other severe infections to take hold, including tuberculosis, oral, lung and liver cancers, and fungal infections.
People living with HIV experience a greater risk of disability, mobility challenges, and cognitive issues, Murzin said. These challenges affect their quality of life and without assistance or proper care, the mental and physical health of those with HIV can deteriorate as a result, said Murzin.
In an email sent on Wednesday, Ken Miller, executive director of the Canadian AIDS Society, told CTVNews.ca there is a "fear" among people dealing with HIV and the type of care they receive.
"Generally speaking, medical staff are not being trained properly in the complexities of caring for people living with HIV and support workers are usually trained even less," Miller said.
In 1997, Canada rolled out antiretroviral therapy (ART) for HIV, allowing people to live with the virus. A previous study published in 2015 explained Canadians undergoing ART had their lifespan climb to 65 years of age. This represents an increase of 16 years since 2000.
With more HIV patients living into older adulthood, care for those who are aging with HIV is generally not a focus throughout training, Miller said.
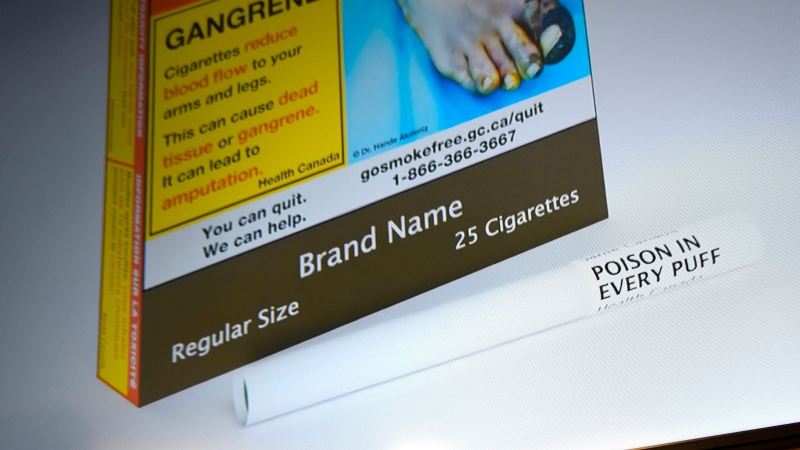
HIV can be spread through sexual activity or by sharing needles or syringes. In advanced stages, HIV can lead to acquired immunodeficiency syndrome (AIDS), which leaves the immune system severely damaged. Since the 1980s, when HIV/AIDS was labelled an epidemic, millions have died from AIDS-related illnesses worldwide, according to UNAIDS.
According to Statistics Canada, there was an estimated 62,050 people living with HIV in 2018. In 2020, there were 1,639 newly diagnosed cases, a 21 per cent decrease from 2019, when 2,122 new cases were reported.
Due to the increased lifespan of people living with HIV, the infection can continue to be transmitted. Murzin says streamlining both HIV treatment and aging in one place would help limit the transmission of HIV.
"Right now, people often get their HIV care either from their family doctor, or most commonly from an infectious disease specialist," she said. "But an infectious disease specialist is in no way trained or prepared to provide care for all of the chronic illnesses that people face as they age."
By educating workers on the additional complexities people with HIV face, along with aging, Murzin says other issues could be mitigated as well.
"Before 1996, treatment options were very limited for HIV. So receiving a diagnosis at a time [when]… you were basically told to get things in order because you wouldn't survive more than six months or a year was extremely traumatic," she said.
Not only did HIV patients need to worry about their health, but disclosing their status to others was usually filled with judgment, Miller said.
"Stigma continues to be one of the largest drivers for HIV transmission," Miller said. "When someone is worried about a positive result, it can deter them from reaching out. This is one of the factors that makes the new [HIV testing] initiatives more important."
Realize and other organizations from around the world have gathered to create 10 calls to action to increase the quality of life for older adults living with HIV. With Dec. 1 being World AIDS Day, these organizations say they aim to bring awareness to the challenges people living with HIV, along with the emotions and complexities of aging.
Some key points include low-barrier access to care, healthy living conditions, targeted research and empowerment, a seat at the decision table, combating ageism and considering sexual health a part of overall health.
"The quality of life is comparably better than previous years by far, but it could always get better," Miller said in the email. "Starting with creating a system that supports individuals who are switching incomes at later years and providing at the very least the basics to every individual that needs it. Dental, physical, psycho-socio and housing supports.”