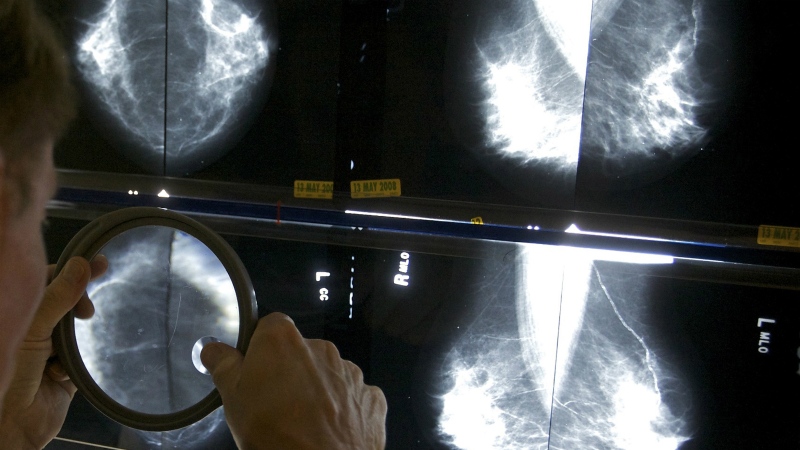
Canada is trailing behind other Organisation for Economic Co-operation and Development (OECD) countries when it comes to both the number of physicians relative to the population, and its spending on primary care, according to a new analysis published in the Canadian Medical Association Journal.
"Health systems with strong primary care have better outcomes, lower costs and better equity," write the nine authors of the study, "Primary care for all: lessons for Canada from peer countries with high primary care attachment."
"Yet, even at the outset of the COVID-19 pandemic, about 17 per cent of people in Canada reported not having a regular primary care clinician."
Meanwhile, the analysis reveals, Canada is seeing declining enrolment in family medicine as a specialty among medical students, and more graduating family physicians are choosing not to practise generalist office-based care. Post-pandemic, 22 per cent of adults in Canada—more than 6.5 million people—don’t have a family doctor they can see regularly for care.
To solve these dilemmas, the authors say Canada should learn from the successes of other OECD countries with high rates of patients enrolled with primary care clinicians.
'WE NEED TO DO THE SAME'
The authors compared Canada to nine countries where more than 95 per cent of people have a family doctor, primary care clinician or place of care—including France, Germany, New Zealand, United Kingdom, Denmark, Netherlands, Finland, Italy and Norway—to find opportunities for improvement here. To make their comparison, they studied data from 2018, 2019, 2020 and 2021.
They found that these countries tend to spend more on primary care, that a greater percentage of their health care is publicly funded, that they have more doctors overall and more of their family doctors are working in family practices. In Canada, by comparison, many doctors work in emergency departments or practice in a specific area, like sports medicine.
Among the nine OECD countries studied, most doctors are paid by salary or a fixed payment arrangement known as capitation, rather than the fee-for-service model common in Canada. They have organized after-hours care and few or no publicly-funded walk-in clinics. They also have smarter information systems that allow doctors to better communicate with patients and allow patients to access their own records online.
While Canada came out in the middle of the pack on health-care spending, the proportion of that spending that was public was the lowest, at 70 per cent. This figure hasn't changed since the 1990s, the study reports.
Canada had similar numbers of family physicians per capita but the lowest number of total physicians per capita by a wide margin, at 24.4 per 10,000 people. After Canada, the country with the second-lowest per capita number was the United Kingdom, with 30 physicians per 10,000 people. Norway had the highest number per 10,000, at 50.4.
Canada also spent less of its total health budget on primary care, and spent more on private health care than any of the other countries studied.
"Other countries have designed their system so that everyone has access to primary care. We need to do the same," wrote Dr. Tara Kiran, a family physician at St. Michael's Hospital and Unity Health Toronto in a media release.
"At the core, we need to guarantee access to primary care and increase how much we spend on it."
AREAS FOR IMPROVEMENT
To bring Canada up to speed with the OECD countries providing the best primary care, the authors say public health care here needs some important updates.
For one thing, most doctors in Canada are private contractors with "little system accountability," they said, whereas the authors say they need to be bound by stronger contractual agreements and accountability to government, insurers or both. They also call for changes to the way health-care providers are paid, specifically to move primary care physicians to capitation or salary payments and away from fee-for-service.
They recommend that a higher proportion of the total health budget be spent on primary care, with medicare coverage extended to prescription medications, dental care and expanded mental health care. They say Canada also needs more physicians per capita.
"Canada should move to a model where residents are guaranteed access to a primary care practise near their home and ensure that these practices are funded appropriately," they write.
Finally, they call for improved patient communications systems, more organized after-hours care and fewer walk-in clinics.
They acknowledge that factors unique to Canada, such as its vast geography, diverse population and proximity to the United States and its health-care system, could pose challenges to emulating its overseas counterparts.
However, they say it's already partway there, "with respect to regional funding of physician services by governments, overall health spending" and the way primary care serves as an access point to other parts of the health system.
"Canada can learn from OECD countries such as the Netherlands, Norway, the U.K. and Finland, where more than 95 per cent of people have a primary care clinician," they conclude. "These international examples can inform bold policy reform in Canada to advance a vision of primary care for all."