It sure looked like I had walked into the wrong operating room in the Ottawa General Hospital a few weeks ago. Jammed with at least a dozen surgeons, doctors, interns and nurses in a frenzy of preparations for the next patient, it seemed the wrong place for my modest day surgery.
But the name on the charts was the name on my wristband, so the nurses swung into action. They slapped on a heart monitor, which displayed a wildly racing pulse, a blood pressure cuff, which registered a sky-high reading to reflect my profound phobia of hospitals, and attached a pair of suction cups for respiratory monitoring.
One doctor started the IV, another checked my mouth for intubation and, as an oxygen mask came down, I was told to relax – fat chance of that happening in a place where cutting open my neck was the next item of business.
As the anesthesia took hold, one thought kept running through my mind: This is a helluva fuss for one little mole.
This is a personal observation from inside our besieged and beleaguered health-care system with one notable difference – in this perhaps atypical case, it worked spectacularly well.
In a system bogged down by stories of closed emergency wards, corridors lined with the very sick, code red ambulance failures and a chronic shortage of nurses and family doctors, this is evidence the system can respond quickly when time is the enemy.
In my case, an irritating mole chafing at the collar had me badgering our family doctor to remove it, which he quickly did and sent off for routine testing.
THE VOICEMAIL NOBODY WANTS TO GET
A week later came the voicemail nobody really wants to get – my doctor saying he needed to chat urgently that very day, a very bad sign of something terribly amiss.
His testing revealed a worst-case scenario for skin cancer: Nodular melanoma Level IV. A surgical team would be in touch within a week, he said.
Now, had this mole surfaced in my neck during the peak of the pandemic when doctor visits were on hold or if, like millions of Canadians, I had no family doctor to visit, this diagnosis would likely have been seriously delayed or even left undetected until it was too late.
What happened to me in the following weeks was a marvel of rapid medical efficiency where long waitlists disappeared to access high-demand care in a hurry.
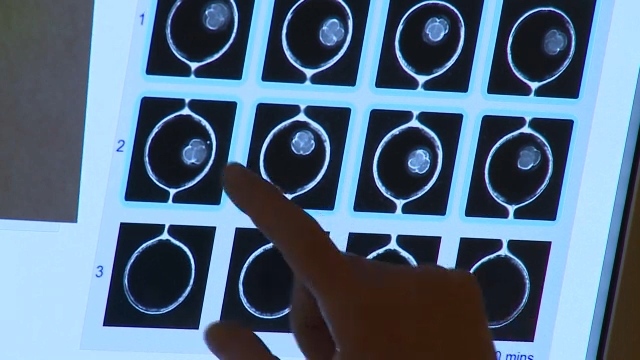
A lymphoscintigraphy led to a surgical consultation followed by an MRI of the brain, with the interesting read-it-one-of-two-ways result that “it didn’t show anything,” and a PET scan within a matter of weeks.
When I remarked that it seemed a very sudden series of treatments, I was told it reflected having a cancer which, once embedding in the lymph nodes, could spread with ruthless speed to the lungs, brain, liver and beyond.
As it turned out, I emerged from anesthesia and intubation to find what I expected would be a pair of smallish incisions to biopsy a few lymph nodes, had become a monster Frankenstein-ish 40-stitch slash from the back of my neck to the throat to allow the removal of four nodes entirely.
As my six-year-old granddaughter Ali marvelled when she studied the scar a few weeks later; “is your head going to fall off Grandpa?”
But the result of such intense scanning and surgery appears to have delivered the best-case scenario – all-clear pathology showing the cancer has not spread into the lymph nodes or beyond.
ONCOLOGIST WILL DELIVER THE FINAL WORD
An oncologist will deliver the final word in the next week or so and regular checks will be in my future, but it appears a potentially dire outcome has been averted.
This success story will be of little comfort to patients trapped without a family doctor to detect it early or access to an acclaimed cancer centre like the one in Ottawa to treat it quickly.
As my surgeon noted when I mentioned I might write up this experience, for every case like mine, others won't have it detected early enough or have timely access to surgery.
No doubt that my little happy-ending story is not the norm, but perhaps it’s not necessarily unique either.
In Canadian health care, it seems, there’s a great safety net. Trouble is, it might not catch you until just before you hit the floor.
That’s the bottom line.