As nurses experience high levels of stress amid increases in hospitalizations for COVID-19 across Canada due to the rapid spread of the Omicron variant, the latest challenge in a two-year struggle against the virus, experts believe organizational changes can help front-line health-care workers cope with burning out.
"Burnout is the end of a very long duration of stress," Nita Chhinzer, associate professor of leadership and organizational management at the University of Guelph, told CTVNews.ca in a phone interview.
"It results in physical, mental, emotional and cognitive depletion of your resources."
There are different methods health-care facilities can employ to aid workers dealing with stress, Chhinzer says, and that responsibility shouldn't be placed primarily on the individual.
"Instead, what we need to do is take a shared responsibility approach to recovery," she said.
"We as a society, we as government officials and public policy makers, as organizational leaders and employers, we need to collectively come together to provide an umbrella of support."
Support can come in the form of programs and protocols that are tailored to specific workplaces with tips and tools coming out of them that are applicable to the job at hand. An example could be the development of escalation procedures, for when workers feel high levels of risk, that put the employee first.
"Health care is one of those interesting spaces where there is a perception that you've got clients and the clients are at risk. We're forgetting that nurses are also at risk," Chhinzer said.
"Nurses, even pre-COVID, were suffering from serious abuse in the workplace."
The tension felt by nurses is an all too familiar story to Doris Grinspun, CEO of the Registered Nurses Association of Ontario (RNAO). A survey put out by the organization in the summer described "an alarming exodus" of nurses leaving the profession as well as high stress levels among peers.
It's a situation that doesn't seem likely to end soon, especially with the emergence of Omicron.
"This virus is not stopping," Grinspun told CTVNews.ca in a phone interview. "Omicron is multiplying exponentially."
She predicts ICUs in Ontario will be full by February, and yet the province will continue to face nursing shortages, partly "because of exhaustion, because they're not treated the way they should, because their workloads are double or triple what they need to be."
Nurses have also reported being stretched beyond their limits, which they say may compromise the quality of care for patients and potentially result in mistakes that could have devastating consequences.
Propping up front-line workers is essential to a functioning health-care system.
Chhinzer points out that, unlike many other sectors, health care operates under a servant-leadership model.
Under such a model, "front-line workers are the ones that need to be supported. Not the manager, not the supervisor," she explained. "The supervisor's job is to provide support to that front-line leader."
But those front-line leaders may now be fewer in number. One potential problem with nurses leaving the health-care system in droves is there may be fewer experienced workers available to mentor new recruits, which can have a cascading effect.
The survey conducted by RNAO also identified the industry's struggle to retain young nurses, some of whom stated an intention to leave at the end of the pandemic. One of the keys to keeping young nurses on board, Grinspun says, is ensuring there are veteran colleagues available to coach them.
"We need [nurses to stay] because we need them to mentor the new ones," she said. "When you come out of school as an RN, you have a lot of fantastic book knowledge, but you need mentors in the workplace to help put that book knowledge into practice."
Losing nurses at an early stage in their career can have a lasting effect on health-care systems.
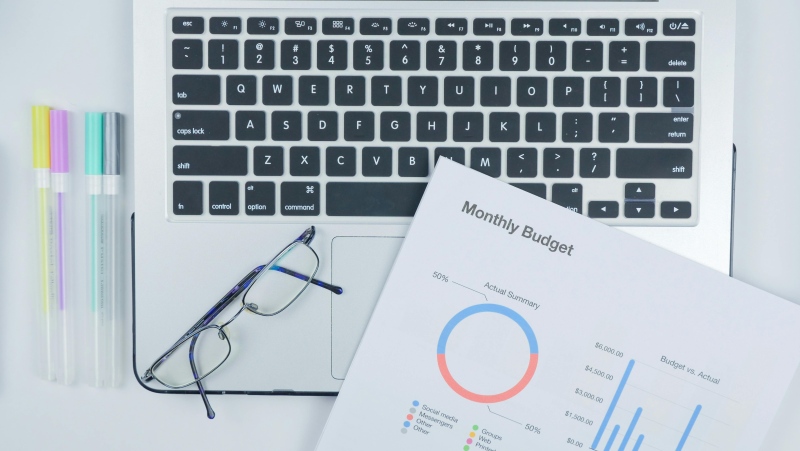
Finally, there's the matter of financial compensation. Many people enter nursing because they have a compulsion to help the sick and wounded, Grinspun says, but it's also a business.
"I can tell you we have that thing in our stomachs. That is an urge," she said. "I hear an ambulance coming, and you know what I want? To go there and help.
"People call it a calling. I don't like to call it a calling because it's a profession and because it's an occupation."
Grinspun has taken issue with Ontario's Bill 124, which caps wage annual increases for nurses at one per cent. The bill was introduced by the provincial government in 2019.
She believes actions such as repealing the bill and providing nurses fair compensation and necessary supports may encourage some of those who left to come back.
Grinspun says right now nurses feel “abandoned” by the province, adding that Premier Doug Ford and Health Minister Christine Elliot are no longer returning her calls.
Chhinzer says there's an opportunity for organizations to bring back nurses who may still feel attracted to the altruistic side of health care if they take initiative and establish support infrastructures.
"While people may burn out and then choose to leave, they're choosing to leave because they feel that they're trapped," she said. "They feel that they have no other choice, but a lot of them still have that true, giving nature in them."
Trying to figure out what caused workers to leave in the first place and offering real solutions may be integral to keeping them in the fold.
"We need to be sure that we are actually following through and that it's not just lip service," Chhinzer said.