Almost half of all Ontario seniors who visited a family doctor for a respiratory infection in 2012 received an unnecessary prescription for antibiotics, a new study has found.
The study from researchers at the Institute for Clinical Evaluative Sciences, and Lawson Health Research Institute in London, Ont. looked at more than 185,000 Ontarian seniors over the age of 65 who went to see a primary-care physician for a non-bacterial upper respiratory infection.
All had infections not caused by bacteria, such as the common cold, acute bronchitis, sinusitis or acute laryngitis. For all these infections, antibiotics would not be appropriate.
The researchers found that approximately 85,500, or 46 per cent, were prescribed an antibiotic. The results appear in the Annals of Internal Medicine.
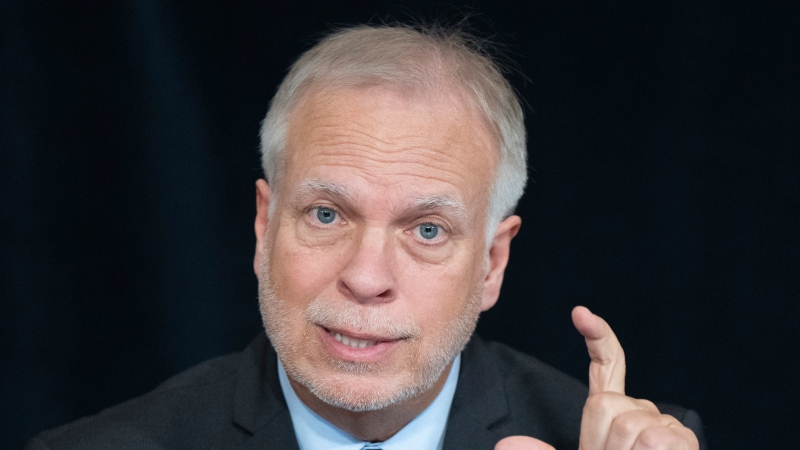
Study author Dr. Michael Silverman, a Lawson scientist and chief of Infectious Diseases for London Health Sciences Centre and St. Joseph’s Health Care, says the finding was not surprising and similar results would likely be found across Canada.
“We don’t think that it’s just particular to Ontario. The same thing has been found in the U.S. and Europe,” he told CTV News Channel on Tuesday.
He noted the study was a thorough one because the researchers were able to look at all seniors who visited doctors for non-bacterial respiratory infections in 2012.
While the study didn’t look at why each doctor chose to prescribe medications the seniors didn’t need, the study points to some interesting trends.
It found, for example, that family physicians who are busier and who were seeing more patients per day were more likely to write antibiotic prescriptions.
“Physicians who were mid-career or later in their career were more likely to write the prescriptions,” he added.
Physicians who were trained outside Canada or the U.S. were also more likely to write the prescriptions, while younger graduates from Canada were less likely.
Silverman says there are lots of reasons why the over-prescription of antibiotics is a problem – most notably because it contributes to antibiotic resistance.
“Antibiotics are a limited resource and we can only continue to use them as long as we save that resource,” he said. “So if we are giving them widely to people who likely don’t need them, then they won’t be around for when we do.”
As well, he added, antibiotics can have serious side effects that are often underappreciated. Macrolide and quinolone antibiotics, for example, can create serious interactions with other medications, and, since many seniors are taking many medications, that can be a huge issue.
Silverman says what’s needed for things to change is to let go of the idea that antibiotics should be taken for all infections, “just in case,” or that a doctor’s visit that doesn’t result in a prescription is a wasted visit.
“We really do have to change our culture,” he said. “The point of going is not to get a prescription. The point in going is to find out what you need and what you don’t need.”