EDMONTON -- A professor of medicine at the University of Alberta says he has discovered proof of a connection between human betaretrovirus infection (HBRV) and an autoimmune liver disease called primary biliary cirrhosis.
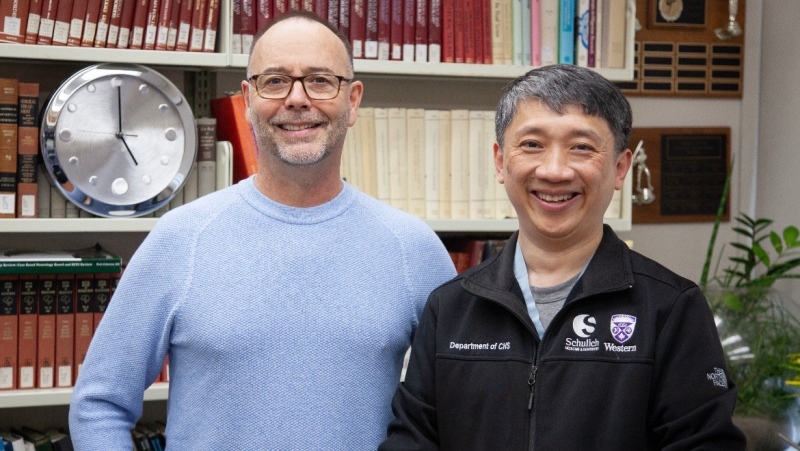
Andrew Mason has published his findings in the February edition of the journal Alimentary Pharmacology and Therapeutics.
Mason says he held fast to his theory for the last decade, even though much of the world's scientific community had long dismissed it.
Primary biliary cirrhosis is a rare disease that affects the bile duct in the liver.
It occurs in one in 500 middle-aged women and is found in about 10 per cent of all patients needing liver transplants.
Despite the progress being made, Mason says HBRV has still not yet been fully linked as the cause of disease.
"Our publication shows that this virus inserts its DNA into the human genome, where we found the junction regions of virus integration in cells of the biliary epithelium, the site of disease," explains Mason, whose colleague in the research was Prof. Gane Wong of the University of Alberta.
"This is the gold standard for demonstrating retrovirus infection. We actually saw over 1,500 unique virus integrations in patients' samples. So that settles an ongoing debate since the 1970s saying that a betaretrovirus like ours is not a human pathogen."
Mason says the discussion reached a stalemate in the 1980s and was eventually ignored once the HIV epidemic emerged.
In 1998 the University of Alberta researcher began examining HBRV and its connection to primary biliary cirrhosis, eventually publishing findings linking the two in the journal Proceedings of the National Academy of Science.
The findings, though, were called into question after another group was unable to find the virus within the liver of PBC patients and challenged the study.
Now more than a decade later, Mason says his team is able to offer further and more detailed proof through the advancement of technology and the use of gene sequencing.
"We always thought that autoimmune diseases like PBC looked like virus infections underneath the microscope but people have been unable to find viruses. Because they found autoantibodies they assumed they were autoimmune diseases. But patients with hepatitis C virus make autoantibodies and no one calls this an autoimmune disease. So we are taking the same approach with PBC as with hepatitis C virus infection. Try and knock out the virus with antiviral therapy."
His team is in the midst of a randomized controlled trial that he hopes will provide further proof. They are following PBC patients who are taking antiretroviral therapy to see if they show clinical improvement.
"Loss of virus equals loss of disease. We have to show that."
Mason believes the findings offer new avenues of research for future clinical treatment. While answers won't come quickly, he says they are emerging, offering hope to patients suffering from PBC.
"We've seen some improvement in patients with recurrent PBC following liver transplantation using antiviral therapy."
Research funding was provided by Canadian Institutes of Health Research, Alberta Heritage Foundation for Medical Research, Alberta Cancer Foundation, Canadian Liver Foundation, Alberta Health Services and the Li Ka Shing Institute of Virology.