It was almost two years ago I placed my first call to Arvin Minocha to hear his story.
A producer at CTV’s ‘The Social’ had passed me his name after hearing I had abruptly lost my younger sister during a nightmarish 24 hours in 1997. Kelly had collapsed at work in Mississauga (she was a cop) and in hospital suffered multiple seizures over several hours, later attributed to a brain tumour she didn’t know she had. I had arrived at her bedside too late, not being able to scramble fast enough from where I was living in New York.
The same thing had happened to Arvin, and his sister Pamela. He couldn’t get to a Toronto hospital in time to say goodbye as her condition rapidly deteriorated. She had been admitted to St. Joseph’s Medical Center with dizzy spells and poor breathing after a dentist’s appointment, dying shortly after from cardiac arrest.
In the aftermath of my family’s loss, we closed ranks and grieved as privately as we could. We never questioned the hospital’s actions over Kelly’s death, wouldn’t allow an autopsy, and never met with any of the staff who had been in charge of her care. Our shock immobilized us. In retrospect I wish we had had the wherewithal to probe the quality of her care more precisely.
Arvin and his family, while just as profoundly saddened by Pamela’s loss, instead started asking some hard questions right away. Ten, to be precise, which Arvin’s friends in the medical community helped him draft. He sent them to St. Joseph’s and within a month received a reply. Not the detailed answers Arvin was hoping to receive to his questions, but a reply.
Arvin isn’t the kind of guy to give up easily.
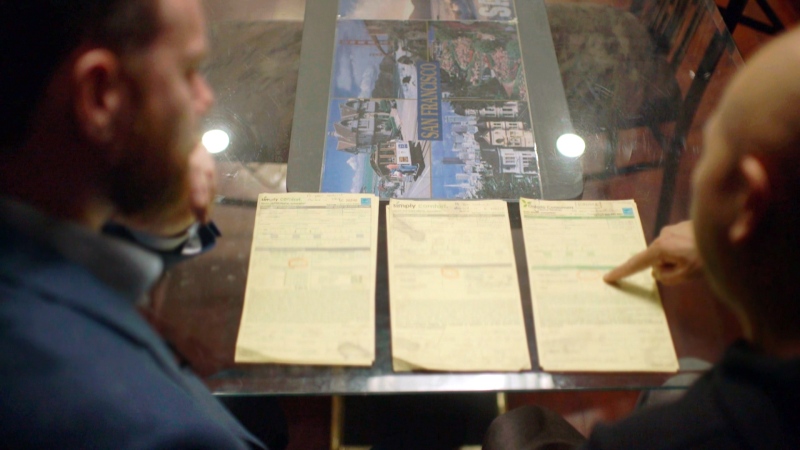
The hospital’s reluctance to move beyond carefully crafted and sometimes vague statements aroused his suspicion. So over the next year, in phone calls and emails (the hospital counted seventy-nine engagements) Arvin relentlessly probed what decisions had been made about Pamela’s care and by whom. He believed there were inconsistencies in the medical records (one doctor wrote the family had been consulted before it removed Pamela from life support -- Arvin and his parents deny that ever happened) and a Coroner’s report that recommended St. Joseph’s review some of its procedures raised even more questions.
An internal investigation by St. Joseph’s into how Pamela Minocha had died was completed, but the hospital wouldn’t share it with Arvin because it was protected under Ontario’s Quality of Care Information Protection Act, or QCIPA.
Other provinces have enacted similar laws in the past decade, which prevent anyone outside of the hospital from seeing the results of internal investigations. They are powerful laws since the Freedom of Information Acts can’t be used to force hospitals to share their reports with patients or their families, and it is entirely at the hospital’s discretion whether to invoke the law. That’s what happened in the Minocha case, QCIPA was declared by St. Joseph’s and an entirely legal cloak of secrecy descended on who did what to try to save Pamela Minocha’s life. If mistakes were made, only the hospital knew it. If actions were taken to address systemic issues, only the hospital and its staff knew it.
All the Minocha’s were told was this: “Our review did not identify or uncover any deficits in the clinical care provided to Ms. Minocha.”
Ontario is now proposing amendments to its QCIPA laws, Manitoba has already adjusted its version. There is a growing recognition that in trying to encourage doctors and nurses to come forward by providing them legal immunity to admit mistakes, families have too often been left without answers to ease their grief. Nothing compels a hospital to hide behind the laws, and some don’t, but critics say the legislation has been used by many hospitals to avoid transparency and sharing with the broader society what they’ve learned after bad things happened to one of their patients.
When W5 reached out to St. Joseph’s the Hospital would only respond via an e-mailed statement: ““The facts, findings and recommendations of Ms. Minocha’s case have been shared with the family.”
Arvin and his family don’t agree. After three years of trying to coax the detailed investigation report from St. Joseph’s have given up trying. So now they are taking the hospital, and by extension the QCIPA law to court, arguing it has created an imbalance in power where the institutions of care have too much power to avoid accountability.
In Arvin’s case his frustration has left him with little trust, but no less determination to know the circumstances of his sister’s death. It’s a fight that has become deeply personal to him, and one many other families who have suffered loss will be watching with interest.