Tom Mulcair: Why Pierre Poilievre's plan to work with provinces to reduce barriers is a good idea
As part of its efforts to deal with the serious shortage of nurses and doctors in the province, the Ontario government has directed the colleges of nurses and physicians to streamline entrance requirements for foreign-trained professionals.
That’s the right call.
The professional licensing bodies are creatures of the provincial legislatures. Self-regulation by the professions is the backbone of our system, but the public interest commands that the ultimate authority reside with democratically-elected officials.
Never waste a crisis, the saying goes, and as we slowly exit the seventh wave of the pandemic, serious shortages of medical personnel have turned a spotlight on an overdue reform.
Many of the rules governing credentialing and equivalences between Canadian and foreign graduates are archaic, based on preconceived notions and in serious need of an objective overhaul.
Prior to the French language leadership debate, professional licensing bodies were high on the list of gatekeepers that Pierre Polievre was planning to reel in.
Of course, professional regulation is first and foremost provincial jurisdiction. If Poilievre didn’t know that prior to the Quebec debate his own handlers (dare I say: gatekeepers?) clearly did and he backed away from his more strident posture.
Now, he said, he was going to work with the provinces to help reduce barriers. That, too, is a good idea.
Poilievre was right to make that concession to constitutional reality, but the validity of his core point was made obvious when the government of Ontario issued its recent directives.
THIS IS ABOUT PUBLIC PROTECTION
There’s nothing new in this debate. There’s a joke in Quebec (where over one million people don’t have a family doctor) that the best way to see a physician is to take a taxi. There’s a good chance the driver is a foreign-trained medical doctor.
I was president of the regulatory agency that oversees all of the professions in Quebec. The same debates took place then and, in the meantime, a lot of solid effort has gone into developing objective ways to evaluate training and determine equivalence of diplomas.
The bottom line is that this is about public protection so no shortcuts that could compromise safety should be allowed, even when there’s a shortage.
At the same time, training standards are more and more harmonized and while safety is the top concern, there’s still a lot of institutional bias in assessing foreign-trained medical professionals.
DON’T PENALIZE FOREIGN GRADUATES
We tend to forget that professional regulation isn’t only about entering a profession. It’s also about inspecting and supervising professionals once admitted. An entire disciplinary process caps the system to ensure respect of patients, standards of practice and rules of ethics.
Yes, we should supervise all professionals. No, we shouldn’t penalize foreign grads by suggesting that letting them in exposes the public to greater harm. They’ll be subject to the same rigorous supervision as all other members of the profession.
I recall a heated discussion between one of the officers of our regulatory agency and a senior player from the college of physicians. It turned on the quality of foreign grads and their training.
My colleague asked a simple question: if you’re travelling in Europe and have a heart attack will you refuse treatment in a local hospital? The answer, of course, was no. Why then all the barriers to integrating those same doctors who choose to move here?
There are arguments that have to do with credentialing: could letting in foreign practitioners dilute the overall evaluation of Canadian graduates and hurt their chances to get licensed in the United States, for example?
These issues are easily dealt with and shouldn’t be used as a shield to prevent foreign graduates from helping to provide the health care Canadians need and deserve.
Similar to Canada, in the U.S., professional regulation is considered a jurisdiction of the individual states: a subset of their policing and lincensing powers. They continue to have many barriers to interstate credentialing and the recognition of professionals.
Here in Canada, we’ve done a decent job of facilitating interprovincial recognition of professionals, though some needless hurdles remain here as well.
I was the first Canadian elected to the Board of the Council on Licensure, Enforcement and Regulation in the U.S.
It was soon after the signing of the original NAFTA. That treaty had the effect of reducing barriers to professional mobility between Canada and the U.S. The only restrictions allowed from now on would have to be competency based. Clearly and transparently.
WHAT WE NEED IN CANADA
Many states still had rules that required you to have taken your licensing exam in the state where you wanted to practise. For example, back then, a New York pharmacist had to be physically seated in Florida when they wrote the licensing exam, if they hoped to practise there. That had everything to do with protecting Florida’s pharmacists from competition and nothing to do with public protection.
Many of those unjustifiable interstate rules were swept away by an international agreement that required an objective look at the motive for restrictions. If a requirement wasn’t about competency and public protection, how could it be maintained?
It’s that type of objective analysis of restrictions and prerequisites that we need here in Canada now.
A second set of professional barriers should be under that objective microscope right now: the scope of practice rules between various health professions. The border line between what one professional can do and what requires membership in a different profession is often fraught and can compromise the ability to do the only thing that matters -- helping the patient.
My brother and I spent a good part of the weekend with our mother in a small regional hospital emergency ward. The care was top-notch but at one point the physician said he’d have to wait another hour before being able to stitch up the leg my mom had injured in her nursing home.
The LPN who was assisting explained that she was allowed to install one type of line and inject this substance but not that medication. That required an RN and none was available. The clock was ticking because stitches had to go in within a certain time after the accident.
All went well in the final result but the question that came to me was: is this barrier between professions really, objectively necessary? Or is it a relic from past arbitrations between professional bodies?
We should take advantage of the current context to insist that governments and professional bodies undertake a concerted effort to:
- Reduce barriers to recognition of foreign professionals;
- Develop objective ways to evaluate diplomas and experience.
- Review restrictions between professions, to improve care.
Tom Mulcair was the leader of the federal New Democratic Party of Canada between 2012 and 2017
IN DEPTH

'One of the greatest': Former prime minister Brian Mulroney commemorated at state funeral
Prominent Canadians, political leaders, and family members remembered former prime minister and Progressive Conservative titan Brian Mulroney as an ambitious and compassionate nation-builder at his state funeral on Saturday.
Trudeau, key election players to testify at foreign interference hearings. What you need to know
The public hearings portion of the federal inquiry into foreign interference in Canadian elections and democratic institutions are picking back up this week. Here's what you need to know.
Who is supporting, opposing new online harms bill?
Now that Prime Minister Justin Trudeau's sweeping online harms legislation is before Parliament, allowing key stakeholders, major platforms, and Canadians with direct personal experience with abuse to dig in and see what's being proposed, reaction is streaming in. CTVNews.ca has rounded up reaction, and here's how Bill C-63 is going over.
As Poilievre sides with Smith on trans restrictions, former Conservative candidate says he's 'playing with fire'
Siding with Alberta Premier Danielle Smith on her proposed restrictions on transgender youth, Conservative Leader Pierre Poilievre confirmed Wednesday that he is against trans and non-binary minors using puberty blockers.
TREND LINE What Nanos' tracking tells us about Canadians' mood, party preference heading into 2024
Heading into a new year, Canadians aren't feeling overly optimistic about the direction the country is heading, with the number of voters indicating negative views about the federal government's performance at the highest in a decade, national tracking from Nanos Research shows.
Opinion
opinion Don Martin: Gusher of Liberal spending won't put out the fire in this dumpster
A Hail Mary rehash of the greatest hits from the Trudeau government’s three-week travelling pony-show, the 2024 federal budget takes aim at reversing the party’s popularity plunge in the under-40 set, writes political columnist Don Martin. But will it work before the next election?
opinion Don Martin: The doctor Trudeau dumped has a prescription for better health care
Political columnist Don Martin sat down with former federal health minister Jane Philpott, who's on a crusade to help fix Canada's broken health care system, and who declined to take any shots at the prime minister who dumped her from caucus.
opinion Don Martin: Trudeau's seeking shelter from the housing storm he helped create
While Justin Trudeau's recent housing announcements are generally drawing praise from experts, political columnist Don Martin argues there shouldn’t be any standing ovations for a prime minister who helped caused the problem in the first place.
opinion Don Martin: Poilievre has the field to himself as he races across the country to big crowds
It came to pass on Thursday evening that the confidentially predictable failure of the Official Opposition non-confidence motion went down with 204 Liberal, BQ and NDP nays to 116 Conservative yeas. But forcing Canada into a federal election campaign was never the point.
opinion Don Martin: How a beer break may have doomed the carbon tax hike
When the Liberal government chopped a planned beer excise tax hike to two per cent from 4.5 per cent and froze future increases until after the next election, says political columnist Don Martin, it almost guaranteed a similar carbon tax move in the offing.
CTVNews.ca Top Stories

'They needed people inside Air Canada:' Police announce arrests in Pearson gold heist
Police say one former and one current employee of Air Canada are among the nine suspects that are facing charges in connection with the gold heist at Pearson International Airport last year.
House admonishes ArriveCan contractor in rare parliamentary show of power
MPs enacted an extraordinary, rarely used parliamentary power on Wednesday, summonsing an ArriveCan contractor to appear before the House of Commons where he was admonished publicly and forced to provide answers to the questions MPs said he'd previously evaded.
Leafs star Auston Matthews finishes season with 69 goals
Auston Matthews won't be joining the NHL's 70-goal club this season.
Trump lawyers say Stormy Daniels refused subpoena outside a Brooklyn bar, papers left 'at her feet'
Donald Trump's legal team says it tried serving Stormy Daniels a subpoena as she arrived for an event at a bar in Brooklyn last month, but the porn actor, who is expected to be a witness at the former president's criminal trial, refused to take it and walked away.
Why drivers in Eastern Canada could see big gas price spikes, and other Canadians won't
Drivers in Eastern Canada face a big increase in gas prices because of various factors, especially the higher cost of the summer blend, industry analysts say.
Doug Ford calls on Ontario Speaker to reverse Queen's Park keffiyeh ban
Ontario Premier Doug Ford is calling on Speaker Ted Arnott to reverse a ban on keffiyehs at Queen's Park, describing the move as “needlessly” divisive.
'A living nightmare': Winnipeg woman sentenced following campaign of harassment against man after online date
A Winnipeg woman was sentenced to house arrest after a single date with a man she met online culminated in her harassing him for years, and spurred false allegations which resulted in the innocent man being arrested three times.
Woman who pressured boyfriend to kill his ex in 2000s granted absences from prison
A woman who pressured her boyfriend into killing his teenage ex more than a decade ago will be allowed to leave prison for weeks at a time.
Customers disappointed after email listing $60K Tim Hortons prize sent in error
Several Tim Horton’s customers are feeling great disappointment after being told by the company that an email stating they won a boat worth nearly $60,000 was sent in error.
Local Spotlight

Marmot in the city: New resident of North Vancouver's Lower Lonsdale a 'rock star rodent'
When Les Robertson was walking home from the gym in North Vancouver's Lower Lonsdale neighbourhood three weeks ago, he did a double take. Standing near a burrow it had dug in a vacant lot near East 1st Street and St. Georges Avenue was a yellow-bellied marmot.
Relocated seal returns to Greater Victoria after 'astonishing' 204-kilometre trek
A moulting seal who was relocated after drawing daily crowds of onlookers in Greater Victoria has made a surprise return, after what officials described as an 'astonishing' six-day journey.
Ottawa barber shop steps away from Parliament Hill marks 100 years in business
Just steps from Parliament Hill is a barber shop that for the last 100 years has catered to everyone from prime ministers to tourists.
'It was a special game': Edmonton pinball player celebrates high score and shout out from game designer
A high score on a Foo Fighters pinball machine has Edmonton player Dave Formenti on a high.
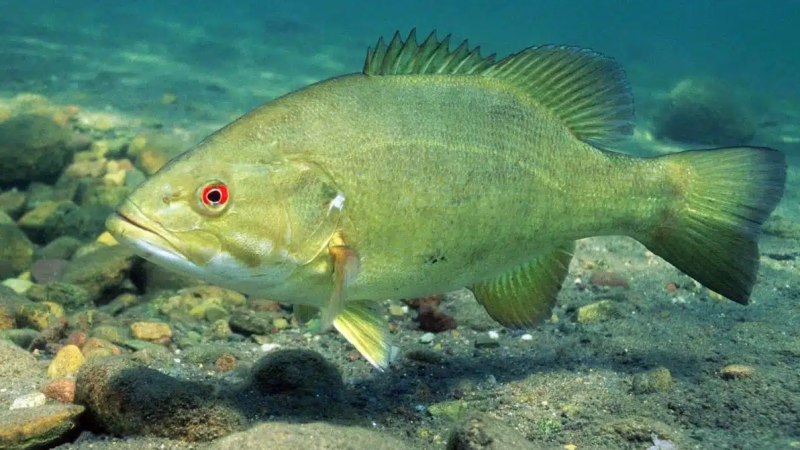
'How much time do we have?': 'Contamination' in Prairie groundwater identified
A compound used to treat sour gas that's been linked to fertility issues in cattle has been found throughout groundwater in the Prairies, according to a new study.
'Why not do it together?': Lifelong friends take part in 'brosectomy' in Vancouver
While many people choose to keep their medical appointments private, four longtime friends decided to undergo vasectomies as a group in B.C.'s Lower Mainland.
Grain-gobbling bears spark 'no stopping' zone in Banff National Park
A popular highway in Alberta's Banff National Park now has a 'no stopping zone' to help protect two bears.
Deer family appears to accept B.C. man as one of their own
B.C. resident Robert Conrad spent thousands of hours on Crown land developing an unusual bond with deer.
Doorbell video shows family of black bears scared off by dog in Sudbury, Ont.
A Sudbury woman said her husband was bringing the recycling out to the curb Wednesday night when he had to make a 'mad dash' inside after seeing a bear.