DEC. 16, 2022 UPDATE: The Liberal government announced it will seek to delay the expansion of Canada's assisted-dying regime to include people whose sole underlying conditions are mental disorders. Justice Minister David Lametti said during a news conference that the government has heard concerns that the health-care system might not be prepared to handle those complicated cases. "Some provinces, territories and those working in the health-care system say that more time is needed," he said.
"It's relief. The relief is what I seek.”
John Scully is an 81-year-old retired journalist. After a 35-year struggle with severe depression, anxiety, suicidal ideation and post-traumatic stress disorder, Scully is waiting to ask for medical assistance in dying or MAiD.
In March 2023, Canada’s MAiD law was going to allow people whose sole underlying medical condition was mental illness to be eligible for an assisted death. But recently the federal government announced they’re seeking an extension before bringing the new law into effect.
"I would probably play some music and I would die peacefully," he told CTV W5. "I don't want to botch it again. I screwed up twice trying to kill myself."
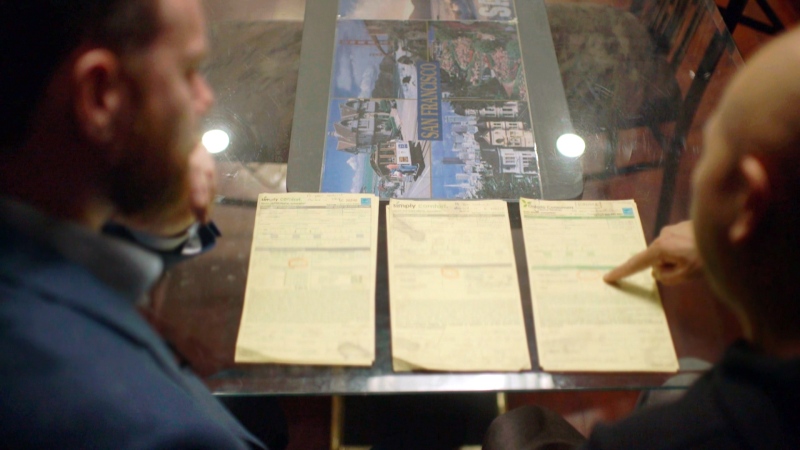
He says he is clear-minded and competent. The evidence is in three books he's written, including "Am I Dead Yet: A Journalist's Perspective on Terrorism."
He’s already started the paperwork for the procedure and has the blessing of his two children and his wife of 57 years, Toni.
Outspoken MAiD provider Dr. Ellen Wiebe wants to help patients like John Scully.
"Mental illness and physical illness both can cause unbearable suffering," says Dr. Wiebe, who’s already provided MAiD to over 400 people with physical illnesses.
Canada’s Supreme Court and federal government are on her and John Scully's side.
A RUSH FOR THE DOORS
MAiD became a legal medical procedure in 2016. It was first offered to those with terminal illnesses such as cancer.
In 2021, the law was amended to include non-terminal physical conditions such as chronic pain. Mental illness was initially excluded to give the government more time to come up with safeguards, which an expert panel of psychiatrists recommended in May of 2022.
Just like for physical illnesses, Canadians with mental disorders will need to show "grievous and irremediable" illness, suggesting their mental condition was incurable, with an advanced state of decline and intolerable suffering.
Two assessors need to confirm the request. And the patient must be found to be competent to make the decision, with a minimum 90-day assessment period before death is provided.
Dr. Wiebe says that more than 1,700 Canadian doctors and nurse practitioners now have six years of practice in assessing suffering patients with physical illnesses.
When assessing someone with a mental illness, she feels the questions are the same.
"Do they understand their disease? Do they understand the prognosis? Do they understand their choices?”
Under the recommended safeguards, people with mental illnesses will also have to show that they have "seriously considered" other treatments, but can refuse those treatments if they find they’re unacceptable.
John Scully would likely qualify.
“I've tried every single so-called cure," says Scully from his Toronto apartment.
He has been hospitalized seven times, been on multiple medications, undergone counselling and has had 19 treatments with electroconvulsive therapy (ECT) that sends shocks to the brain to lift depression. He is now on 30 pills a day to try to manage his chronic pain and health problems.
He's not alone.
CTV’s W5 spoke with several Canadians with long-standing mental disorders who welcome the imminent change.
"There's going to be a rush for the doors," says Mitchell Tremblay.
The 40-year-old says he was diagnosed with severe depression as a teen and he also deals with anxiety, alcoholism, personality disorders and continual thoughts of suicide. He can’t work and lives in poverty on a disability payment of just under $1,200 a month.
"You know what your life is worth to you. And mine is worthless," he says.
STATE SANCTIONED SUICIDE

But some experts warn Canada is about to offer what they say will amount to "state-assisted suicide" for the mentally ill, at a time when health services are strained.
At the regular morning meeting at the Canadian Mental Health Association offices in Barrie, Ont., a team of social workers and nurses and psychiatrist John Maher discuss the people they are trying to help. A big part of their work has been suicide prevention.
"I had a patient who talked to me recently about MAiD who wants to die because of his belief no one will ever love him," Dr. Maher told W5.
He says colleagues have shared similar stories of patients in their care, enquiring about how to stop therapy and qualify for assisted death.
Dr. Maher says, “the wait times for our treatment programs in Ontario are up to five years.”
"There are cycles of illness... Some of it's up and down. It might be years. And then there's a burst of illness and suffering that we then take care of,” says Dr. Maher.
MAiD for mental illness is too close to suicide for his comfort.
“You're assisting someone in the completion of their suicide. The doctor is the sanitized gun," says Dr. Maher. One of his key concerns is how anyone can determine if someone with a mental illness is incurable, as is required by the legislation.
"I'm not at all disagreeing that there are people who have an irremediable illness. What I defy you or any other person in the universe to prove to me is that it's this person in front of you.”
AFRAID OF DYING BY MEDICAL ASSISTANCE
Serena Bains says all this talk about MAiD for psychiatric disorders has only heightened her thoughts of suicide.
The 24-year-old who lives in Surrey, B.C. has severe depression, anxiety and borderline personality disorder. She was hospitalized once when she told a doctor she was planning her suicide.

But despite her "disabilities" as she calls them, she's completed a university degree and is preparing to start a new internship in Ottawa.
Her worry is that if she spirals downward and hits a rough patch she might be suicidal enough to ask for MAiD and qualify.
"A lot of the conditions I have ... they're perceived as being severe. They've been consistent. I've had them since I was a teenager," she says.
Serena’s been on a waitlist to see psychiatrists multiple times. "This year it took, like, a year and three months," she tells W5.
Studies confirm that there are long waits for mental health care across Canada. One in 10 Canadians looking for counselling services wait more than four months. It’s even longer for children and youth. Serena says the mental health system is broken.
"It's not consistent. And honestly, once they move you to another service, there's usually a waitlist for that," she says.
She wonders why governments don’t offer more mental health services before making MAiD widely available.
"More accessible health care, more psychiatrists should be available, more forms of therapy should be available.”
Not only are there long waits, people with mental disorders often face problems with access to health care, housing and food. According to the Canadian Mental Health Association, 70 to 90 per cent of people living with serious mental illnesses in Canada are unemployed.
Although MAiD accessor Dr. Ellen Wiebe says there are weaknesses in the mental health system and wait times are too long, it doesn’t mean patients shouldn’t necessarily be eligible for assisted death.
"Would I like there to be better mental health treatments in this country? Yes, of course. But if delays in care cause irremediable pain, it is still suffering."
Canadians are also questioning whether offering a mentally-ill person assisted dying while they’re awaiting treatment is the right thing to do. A CTV News Nanos poll suggests that 61 per cent -- almost two-thirds of Canadians -- are unsure or don’t support MAiD for those waiting for care.
THE MOST LIBERAL IN THE WORLD
As it stands right now, bioethicist and Washington based psychiatrist Dr. Scott Kim says Canada is about to become the most liberal country in the world in allowing those with mental disorders to access assisted death.
Dr. Kim has been studying psychiatric euthanasia and its use in countries such as Belgium and the Netherlands, where it’s been practised for two decades.
Both countries have more stringent requirements for proving an illness is irremediable, says Dr. Kim, by requiring psychiatric input and putting more emphasis on trying additional therapies than is recommended in Canada.
Belgium also has a two-track system in which patients and doctors look for potential therapy and treatments, while another team assesses the patient for MAiD.
The rates of approval for psychiatric illnesses in Belgium and the Netherlands are low, says Dr. Kim, ranging from just one to three per cent.
“The large majority are rejected,” he says. "Overwhelmingly, the main reason is there are other alternatives."
In Canada, there’s some disagreement about whether patients who want assisted dying need to try treatments or only that they must be informed of what is available.
Dr. Ellen Wiebe says health care professionals who provide MAiD are careful to review the treatments the patient has undergone, though more treatments can’t be forced on anyone.
“Individually, assessors will look at what treatments they have received and say you haven't tried this or this or this…and then the patient would have to convince me that there was a good reason not to try them.”
CANADA UNDER THE MICROSCOPE
Canada has already been under the international microscope for its increasing use of medically-assisted death for physical disorders. The latest Health Canada report shows a steady increase over the past six years to where 3.3 per cent of all deaths in 2021 were from MAiD. That has quickly approached the European average where about four per cent of all deaths are assisted deaths.
"I've had colleagues call me from other countries saying, you know what's going on in Canada?” says MAiD skeptic Dr. John Maher.
But Dr. Wiebe argues the new rule acknowledges the plight of those suffering from intolerable mental illnesses.
"If you are suffering unbearably, you've got the right to say, 'I've had enough' and you'll go through a process with safeguards,'' says Dr. Wiebe.
John Scully agrees. MAiD promises him relief from almost four decades of mental suffering. But its arrival also makes him sad.
"It just formalizes the utter failure of psychiatric medicine," he says.
Kevin O'Keefe is W5 producer for 'The Death Debate'. Watch the episode on our player at the top of the page