After a B.C. man living in a care home became the first person in Canada to die while battling COVID-19, officials in B.C. are outlining the extensive challenges these facilities are facing in this outbreak, including staff and supply shortages, as well as concerns over family visits.
Daniel Fontaine, CEO of B.C. Care Providers Association, told CTV’s Your Morning that visitors are not banned, but care homes in the province are asking family members to stay away, if possible, and screening those who do visit.
“We’re putting in a number of different protocols,” Fontaine said. He said that visitors are being asked “whether or not they’re in any way symptomatic, and if they are, we’re asking them to leave.”
A man in his 80s who was residing at North Vancouver’s Lynn Valley Care Centre died on Sunday, a day after he was confirmed to have the novel coronavirus.
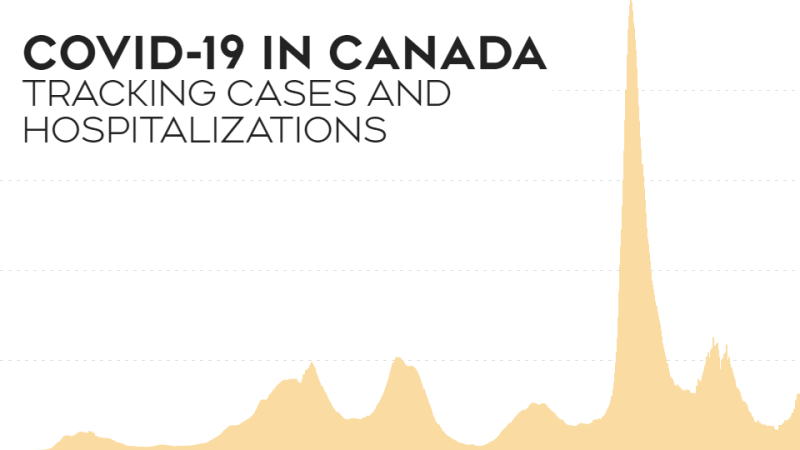
Another resident, a woman in her 70s, also was confirmed to have the virus on Saturday. She is in stable condition. So far, Canada has 80 confirmed cases of coronavirus, but the B.C. man is the first death.
Fontaine said that they have some systems in place from responding to influenza outbreaks -- such as ensuring extra cleaning of all rooms and wiping down all surfaces -- but that the scale and intensity of the response to coronavirus is “more enhanced.”
He said that they were “really encouraging people,” to refrain from visiting care homes over the next few weeks.
“If you do come at the moment, you’re still allowed to come in, but you will be asked some questions, and you’ll be, in many cases, asked to just strictly go to visit your loved one, not visit any of the common areas, (to) help prevent the potential inadvertent spread of COVID-19.”
In remarks about the outbreak, many health officials frequently remind the public that most cases of the virus are mild. While true, that rhetoric can downplay the perception of risk to elderly or immunocompromised individuals, who face a significantly higher rate of severe illness or death if they contract the virus.
Ontario’s chief medical officer of health Dr. David Williams stressed at a news conference on Monday that the general public should be careful with practising hand-washing diligently and staying at home while ill so that “you can protect … that population at risk.”
The impact on residents in care homes is a national concern, particularly in light of the death at Lynn Valley Care Centre.
Ontario’s health ministry said Monday that anyone going in and out of a care home -- including staff, visitors and volunteers -- would be asked about travel history and checked for symptoms.
The province will also be testing for COVID-19 at any long-term care facilities where there has been any form of respiratory illness.
Nova Scotia’s chief medical officer of health, Robert Strang, said in a news conference Monday that anyone who had travelled outside of Canada should not visit nursing homes within 14 days of returning to Canada.
"In that 14-day period, even though you're healthy, do not come and visit in a long-term care facility,” he said. “We need to do everything we can do to prevent the introduction of this virus into a long-term care facility setting."
However, cutting down on family visits has its own drawbacks.
Laura Tamblyn Watts, policy director at the National Initiative for Care of the Elderly (NICE), said that one of the challenges was the mental and emotional toll of isolation.
“When you have older people who are at risk of social isolation -- it's very upsetting for them to be in isolation in many instances,” she said.
“And if you have people with cognitive impairment, they may not understand why no one is coming to visit them."
External visits from potentially infected family members are not the only challenge facing officials at care homes.
One of the drawbacks of mass public panic over the virus is the surge in demand for “things like surgical masks and gloves and antiseptics and all the stuff that typically the public does not purchase,” Fontaine said.
“So a number of care homes are having challenges with their suppliers, trying to get access to things like medical supplies,” he said. This also increases the risk level during family visits. When there is a flu outbreak in a care home, Fontaine said, staff usually give masks to family members to wear while visiting. Now, they may not have enough in stock to always do that.
And the desire to keep infectious people away from residents means that staff shortages are becoming a serious issue.
Fontaine said that they’ve had shortages particularly in “the interior of British Columbia and on Vancouver Island … with so many staff calling in sick and indicating that they’re not coming in, due to the fact that obviously they want to prevent the spread of COVID-19.”
The cases identified in residents at Lynn Valley Care Centre on Saturday -- including the man who has since died -- were linked to B.C.’s first “community case” of coronavirus, a woman in her 50s who was a staff member at the care centre.
With files from The Canadian Press