TORONTO -- Taking even low doses of opioids like codeine or morphine increases the risk of being involved in a traumatic motor vehicle accident -- and that risk goes up as people take higher and higher amounts of the powerful pain killers, research suggests.
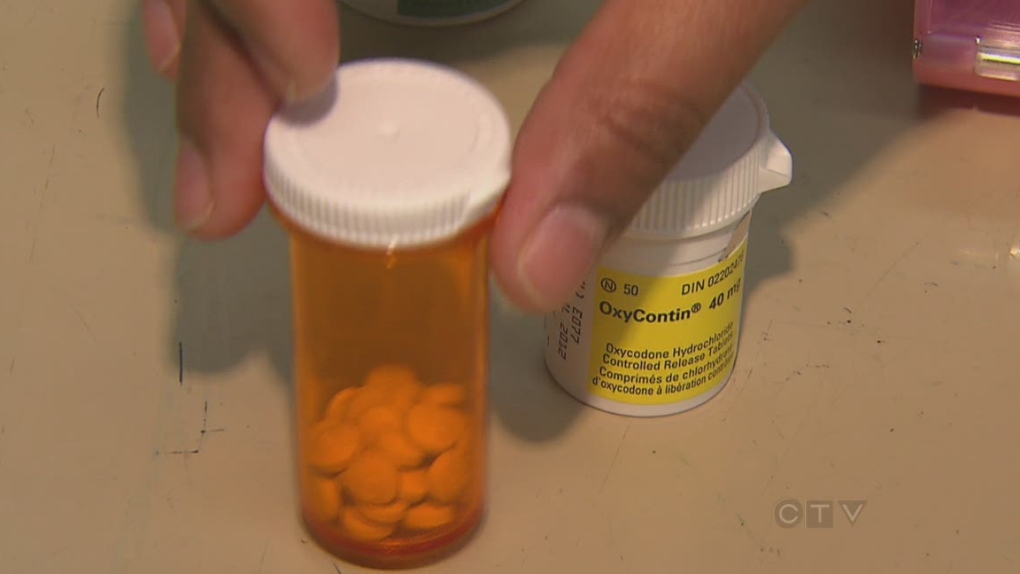
Opioids, the widely prescribed class of drugs that also includes oxycodone, hydromorphone and the fentanyl patch, are prescribed for both acute and chronic pain. The medications can play havoc with alertness and reaction time, especially when people first start taking the drugs or have their dosage raised.
The study, published Monday in JAMA Internal Medicine, found that among adult drivers prescribed opioids, a daily dose of just 20 milligrams of morphine (or the equivalent of another opioid) was linked to a 21 per cent increased risk of road trauma.
The chance of having an accident rose to 42 per cent with "high" doses of an opioid, described as 100 to 199 mg of morphine or its equivalent, compared to low doses of the drug.
"What we found was that the risk of a motor vehicle collision was dependent on the dose of opioid the individual was receiving, this was for people who were driving the car," said Dr. David Juurlink, one of the co-authors of the study by the Institute for Clinical Evaluative Sciences in Toronto.
"I think the most important observation was that even low doses of opioids -- these are doses in the 20 to about 50 milligrams or so per day -- were associated with an increased risk of accidents compared to very low doses," he said.
Meanwhile, those prescribed "very high" doses of an opioid -- more than 200 milligrams per day -- also had an increased risk of road trauma while driving. But at 23 per cent, it was lower than might be expected.
Despite the high-end dose, Juurlink said the risk may be lower because patients taking that level of drug have likely been on the medication for a while and their brains have adjusted to its effects.
Another possibility is that people on very high doses drive less because they're in severe pain, so it only appears that the risk for this group is lower, he said.
"It's also conceivable that some people are not taking but actually selling (the drugs), so that also might attenuate the risk to a certain extent."
Using Ontario prescription data and hospital records, the study looked at almost 550,000 patients aged 19 to 64 who received at least one publicly funded prescription for an opioid from April 2003 to March 2011. The study examined 5,300 of these patients who were treated in a hospital emergency department after being involved in a traffic accident.
While increased risk levels of 21 to 42 per cent may seem modest at first glance, widespread prescribing of opioids means the issue of road safety is an important one, the researchers stress.
"When you think about the hundreds of thousands, if not millions, of Canadians who take these drugs, I think it's fair to say that the use of opioids while driving may constitute a significant and previously under-appreciated public health problem," Juurlink said.
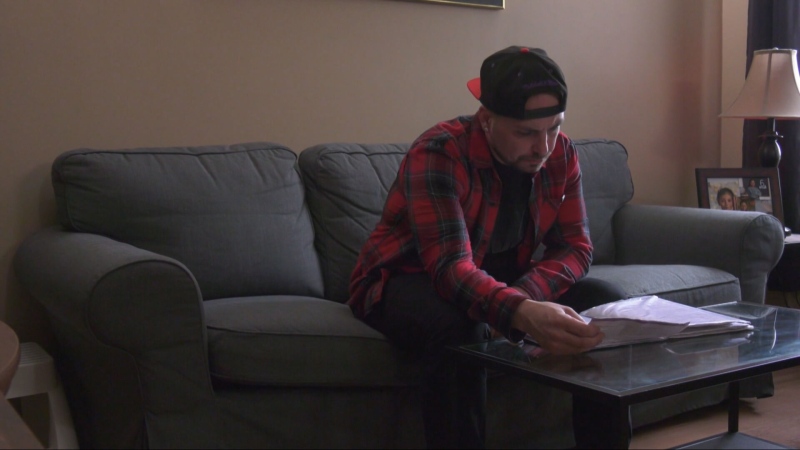
Patients taking the pain killers should consider hanging up their car keys or at least minimizing the amount they get behind the wheel, he said.
Physicians can also play a role in keeping these drivers safe, as well as their passengers, pedestrians and other motorists with whom they interact on the road.
"I think it's incumbent upon docs to warn patients at the time a prescription is written that they should think twice about driving."
In fact, that is one recommendation of the Canadian Guideline for Safe and Effective Use of Opioids, said Dr. Andrea Furlan, who helped formulate the advice for physicians published in 2010.
The guideline recommends that doctors strongly advise patients against driving when they first start taking an opioid or when their dosage is being adjusted up or down.
"But once they reach a stable dose, they can tell the patient 'Now you can go back to driving,"' said Furlan, who was not involved in the ICES study but welcomed its findings.
Furlan, a pain specialist and researcher at Toronto Rehab, said there were virtually no high-quality studies on the potential link between opioid use and road trauma at the time the guideline was drafted.
"This is a piece of evidence that is missing," she said of the ICES study.
Even so, Furlan said because the study is based on administrative records, the findings may be somewhat skewed.
For instance, the data can't reveal whether people prescribed opioids were actually taking the drugs, she said.
"I have a lot of people that I prescribe opioids to for pain. They go to the pharmacy, they fill the prescription, but they come back and say, 'I took one pill, I didn't like (it)."'
As well, patients with chronic pain often take multiple medications, including anti-anxiety and anti-depression agents that can also have sedating effects and could undercut one's ability to drive.
"The other thing that is very important is we know that pain itself affects driving," Furlan said. "Even if it's a headache or menstrual cramps or acute low-back pain or neck pain ... your concentration is impaired, your reaction time is impaired, your attention -- all those things that are important for driving."
The database used by the researchers does not include patients' level of pain, so its effect on driving performance could not be assessed or teased out of the risk equation, she added. The same is true for patients' sleep status.
"A lot of people that have chronic pain, or even acute pain, they don't sleep well. So they are driving with sleepiness because night after night they are not sleeping well. So they are chronically tired."
Still, Furlan said she is not surprised by the study results and hopes planned research to test the driving ability of patients on opioids in a variety of real-time conditions will help elucidate the risk.
"There is a signal here."