When Taylor Binns slowly began going blind because of complications with his contact lenses, he started to prepare for living the rest of his life without vision. But an innovative treatment using stem cells has changed all that, and returned to him the gift of sight.
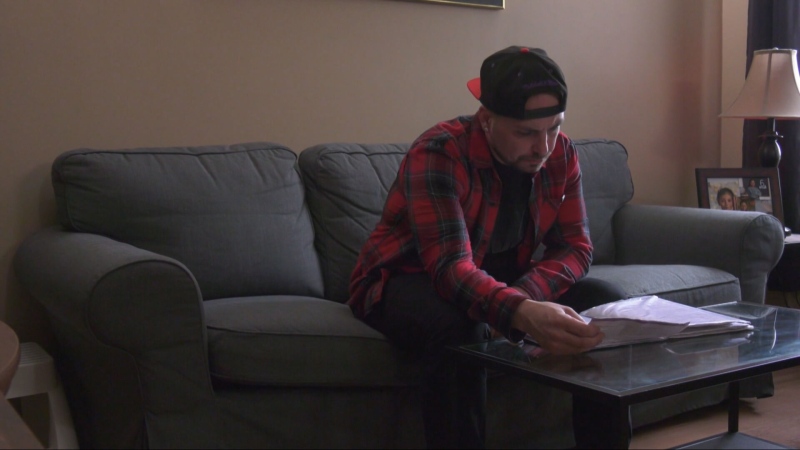
Four years ago, while on a humanitarian work mission to Haiti, Binns developed intense eye pain and increasingly blurry vision. Doctors at home couldn’t figure out what was wrong and, over the next two years, Binns slowly went legally blind, no longer able to drive or read from his textbooks at Queens University, where he was studying commerce.
“Everything you could do before was being taken away, day by day, and it got worse and worse,” he recalls.
Doctors finally diagnosed him with a rare eye disease called corneal limbal stem cell deficiency, which was causing the normal cells on Binns’ corneas to be replaced with scar tissue, leading to painful eye ulcers that clouded over his corneas.
A variety of things can cause the condition, including chemical and thermal burns to the corneas, which are the glass “domes” over the coloured part of our eyes. But it’s also thought that microbial infections and wearing daily wear contact lenses for too long without properly disinfecting them can lead to the disease, too.
Since a corneal transplant was not an option for Binns, hisdoctors at Toronto Western Hospital proposed something new: a limbal stem cell transplant.
The limbus is the border area between the cornea and the whites of the eye where the eye normally creates new epithelial cells. Since Binns’ limbus was damaged, doctors hoped that giving him healthy limbal cells from a donor would cause healthy new cells to grow over the surface.
While the treatment is available in certain centres around the U.S., Binns became the first patient to try the treatment at a new program at Toronto WesternHospital.
Though Binns knew he’d need to take anti-rejection drugs, he decided the procedure was worth a try.
“The alternative was to live in constant pain all my life,” he says. “So there really wasn’t anything to lose.”
Just like with an organ transplant, Binns’ doctors had to find a healthy match. It turned out his younger sister, Victoria, was the ideal candidate for the job.
In the operating room, doctors removed the scar tissue on Taylor's eyes, then took some healthy stem cells from Victoria's eyes and stitched them to the surface of Binns’ eyes.
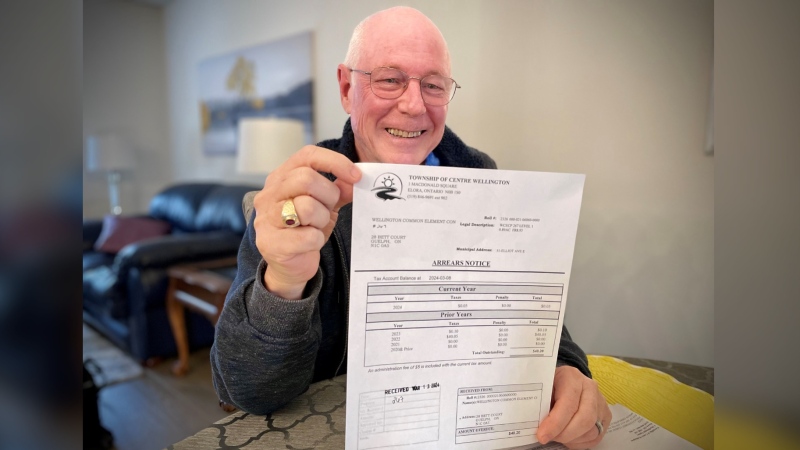
“Within a month he could see 20/40,” says ophthalmologist Dr. Allan Slomovic. “His last visit he was 20/20 and 20/40.”
Slomovic says “it’s extremely exciting” that the procedure was a success, “especially when you realize there is really nothing else that would have worked for him.”
Binns is now living pain-free, returning to doing everything he used to before his three-year sight loss.
“Being able to see my computer, being able to go for a walk or a drive -- I am so happy for that,” he says.
The Toronto team hopes to do many more of these procedures in the future, says Dr. Sherif El Defrawy from the Canadian Ophthalmological Society and University of Toronto’s ophthalmology department.
“We are already seeing this in a number of centres across the country and you will see it more and more as we understand how to improve the success rate,” he says.
Researchers are also working on using stem cells from deceased donors and even using limbal stem cells from a patient’s own eyes. While that would require growing the cells in a lab to force them to multiply, it would also mean that patients might be able to skip anti-rejection drugs.
For Binns, the experience has been life-changing in one more important way: He has now decided to switch his studies from commerce to medicine, and hopes to go to school to become an ophthalmologist.
Toronto Western Hospital has done 6 similar procedures since Binns was treated and all were successful. Most of those patients had suffered burns to their eyes from chemical injuries and some people had been living with birth defects of the surface of the eye.
All stem cell transplants came from a living related donor.
With a report from CTV’s medical specialist Avis Favaro and producer Elizabeth St. Philip