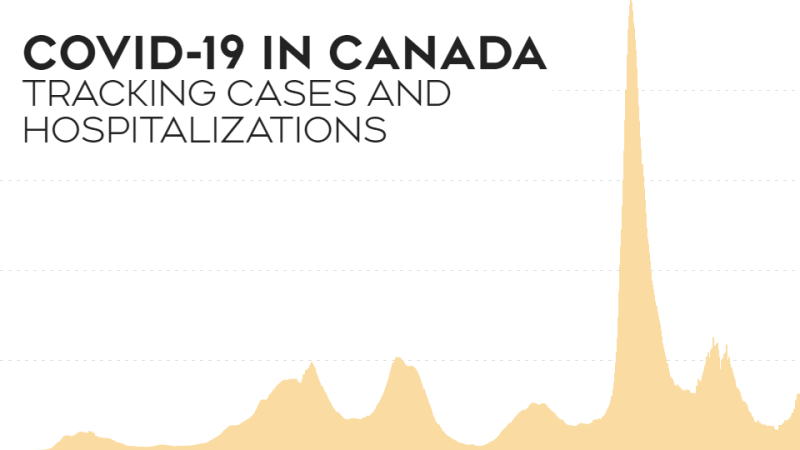
TORONTO -- ICU occupancy in Ontario has hit a record high, and more than 150 doctors have penned an open letter to the province's medical officer of health to stop basing COVID-19 restrictions on available ICU beds.
With a third wave underway and ICU beds filling up, hospitals are having to transfer patients to other facilities to ease some of the load in COVID-19 hotspots, and doctors want new policies in place to curb the spread.
“Ontario is at a critical point in the pandemic, and we are being led down a very dangerous path by using ICU capacity as a benchmark for tolerance of COVID-19 spread. We do not agree with this approach and believe new public health measures are required immediately in order to regain control of the pandemic and save lives,” the letter reads.
The variants of concern are the main driver behind the third wave.
“We certainly see wave three become a particular problem, a particular problem because of the variants of concern, because of the number of patients that are acquiring COVID at a much more rapid rate, and with more severity of requiring hospitalization at a higher rate, leading to increased risk of death,” Dr. Martin Betts, a signatory and medical director of critical care at the Scarborough Health Network, told CTV’s Your Morning
Not only are the variants of concern leading to more COVID-19 infections, but they’re landing more patients in the ICU.
“We know the variants of concern in Ontario double the risk for requiring ICU care with each individual infection,” Betts added.
And the patients ending up in hospital and in ICUs are younger.
“We are seeing younger patients on ventilators—many are parents of school-aged children. We are seeing entire families end up in our ICUs. We are caring for people who have contracted COVID-19 at work, or who have followed all the rules and only gone out for groceries. The impact of this virus has been disproportionate, infecting those with highest exposure risk, commonly from lower income and racialized communities,” the letter says.
Because of the number of COVID-19 patients filling ICU beds, people requiring major surgeries and procedures are having to wait even longer than previously expected. This comes just months after hospitals resumed surgery programs over the summer as case numbers dropped.
Betts said at his hospital, with the ICU at capacity, urgent patients who require critical care are tended to in the post-operative area, forcing other patients to wait.
“That puts back pressure on the surgical programs and means that patients that need potentially life-altering surgery are being asked to wait, and given the most recent rise in cases, we're probably going to have to ask them to wait even longer,” he said.
Even with unlimited ICU beds, the situation is untenable, the letter says.
“Even if we had unlimited ICU capacity, allowing these VOCs to spread exponentially is unethical. About 4 in 10 patients who come to the ICU with COVID will die. More than half of patients requiring mechanical ventilation due to COVID will die. Patients who survive a prolonged ICU admission and are discharged home can have significant long-term impacts on physical or cognitive function.”
This doesn’t mean that should you require urgent care, the hospitals in Ontario won’t be able to provide that care to you.
“For any patient that has an urgent need for medical care, come to the emergency department, we will find the care that you need to care, to take care of your condition,” said Betts.
There’s a system in place in Ontario to keep at least one ICU bed available in Ontario hospitals, but to do so, patients are being shifted around Ontario’s hospital system.
“Last weekend we had five patients and families consent to transition to Kingston and Peterborough to continue receiving their care,” he said. “But the same day we received six calls from other hospitals in the GTA from the west end, from downtown Toronto, from North York region, just within hours, asking if we can refill up those beds with patients having need.”
While Ontario Premier Doug Ford has funded more critical care beds throughout the pandemic, Betts said it’s not enough without properly trained nurses and doctors to staff those beds and tend to the patients in them.
“You can't just print a nurse off a printer and have them come to work the next day,” he said.
It’s not just a lack of beds and properly trained staff causing problems, important supplies are beginning to run low.
“Certain elements of care, for instance tocilizumab, which has been known as a life saving medication for patients with COVID, but we know our supply is quite limited,” said Betts. “And as cases ramp up, it's threatened and we're actually having to start thinking about rationing that life saving medication to patients that have this.”
ICU physicians have been on the front lines of the pandemic since it began, and their workload shows no sign of lessening.
“We frankly are burnt out, and we're seeing too much suffering and concern that having public health policy based upon a COVID-19 transmission tolerance of ‘how many ICU beds do you have left?’ is going to put patients at risk,” he said.