VANCOUVER -- Addiction experts from five European countries say their experience with prescription heroin programs have provided overwhelming evidence to suggest Canada should expand its one clinic in the midst of a deadly opioid crisis.
Researchers from the Netherlands, Denmark, Germany, Switzerland, the United Kingdom and Canada held a symposium in Vancouver on Friday to share lessons they've learned from multiple clinical trials and years of treatment.
Wim van den Brink of the Netherlands told a news conference that some European programs started as a way to deal with the public nuisance of drug use but the medical health benefits improved people's quality of life and saved money in the criminal justice system.
"There's so much experience locally and internationally, the efficacy is so clear," said van den Brink, a professor of psychiatry and addiction at the University of Amsterdam's Academic Medical Centre.
"I'm not sitting here with some kind of moral superiority that we did it so wonderful. Politically, it wasn't primarily motivated by public-health issues."
Seventeen clinics provide supervised injectable and inhalable heroin for about 800 chronically addicted patients in the Netherlands, he said.
The impetus for the gathering, organized by the Public School of Health at the University of British Columbia, was an estimated 2,000 overdose deaths across the country just since 2016, many involving the painkiller fentanyl.
Vancouver's Swiss-based Crosstown clinic is the only facility in North America that provides heroin treatment for people who have committed to two or three supervised injections daily after failing at multiple other interventions.
"Even from a medical perspective, this is a cheap treatment if you can save so many lives," van den Brink said. "The only thing is, do we think the lives of addicts are worth the same thing as people with any other disease?"
Senior research fellow Nicola Metrebian, of the National Addiction Centre at King's College London, said the United Kingdom government funded four clinics providing injectable opioid treatment in 2012 based on evidence from a major clinical trial there and from international research but the facilities were forced to close because of a lack of funding.
"We are in a very similar position to you guys in Canada," she said of evidence of effectiveness and lack of funding. "We are still trying to get this into routine treatment."
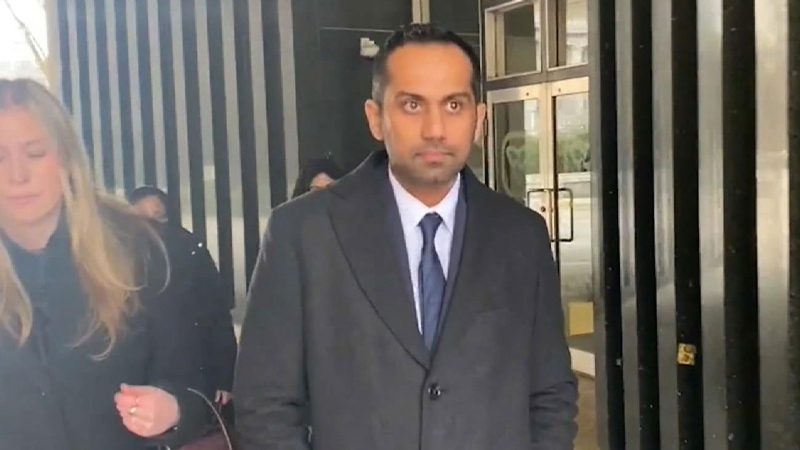
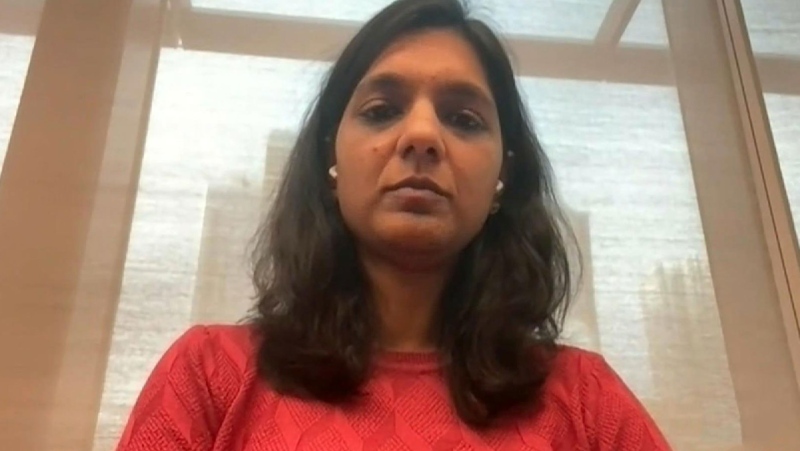
Eugenia Oviedo-Joekes, an associate professor at the University of British Columbia's School of Public Health, presented two major Canadian studies that led to the opening of the Crosstown clinic.
The program that currently provides heroin-assisted treatment to 95 patients has a wait list of up to 600 people and needs to be urgently expanded, she said.
Oviedo-Joekes said people who are treated at Crosstown no longer use deadly opioids sold on the street and get help from social workers with issues such as filling out housing applications as part of a network of support.
She said Denmark used international research, including from Canada, to open its clinics because it wasn't necessary to do any more clinical trials when lives needed to be saved.
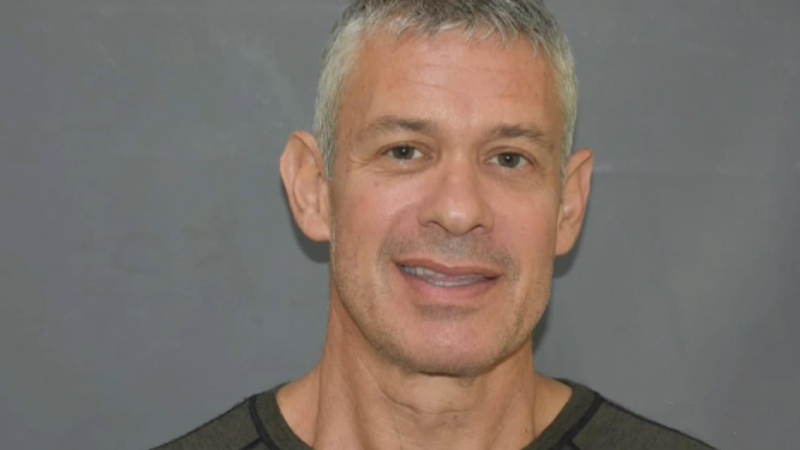
Dr. Martin Schechter, who chaired the Vancouver symposium and has extensive expertise in HIV research, said the federal government has introduced several initiatives during the opioid epidemic, but provinces have balked at paying for programs.
"We're hoping that people here across Canada will see that the sky did not fall in Europe. It's a helpful addition to the treatment system and we have to be more open minded in Canada."
Schechter said evidence from two studies, in Canada and the Netherlands, showed significant cost savings from treating patients with various injectable forms of medication, including heroin.
"So to argue that we can't afford it is wrong. The question is whether we can afford not to do it."
Vancouver Mayor Gregor Robertson said he has repeatedly urged the B.C. government to expand prescription-heroin treatment.
"Crosstown is a living example of a clinic that's keeping people with addictions alive while their friends on the street are dying because they can't access the safe pharmaceutical drugs to start the process of treatment and recovery."