Three new infections with the novel coronavirus have been found in eastern Saudi Arabia, raising questions of whether some person-to-person spread of the virus has occurred there.
The World Health Organization confirmed Friday that it had been informed of the three cases, one of which was a family member of another case which had been reported earlier in the week. The WHO said all three are in critical condition.
Late Wednesday, Saudi Arabia told the WHO it had confirmed seven infections, all of whom had been or were being treated in the same hospital in the Al-Hasaa region. By the time the cases were reported, five of the seven had died and the remaining two were critically ill.
While no additional details were initially available, the Kingdom's deputy health minister, Dr. Ziad Memish, provided information about all 10 on Friday via the Internet-based disease alert system, ProMED-Mail.
The original seven cases in this group all reportedly had "multiple comorbidities." A comorbidity is medical-speak for a disease or condition. The ages of the initial seven cases ranged from 24 to 94, though most were in their 50s.
Infectious diseases expert Michael Osterholm said looking at who became infected may provide clues to how they became infected, calling it striking to see so many people listed as having multiple comorbidities.
"I'd like to know what these comorbidities are. Because there's something that's telling us something there," said Osterholm, who is the director of the Center for Infectious Diseases Research and Policy at the University of Minnesota.
Having a pre-existing medical condition can make people more susceptible to becoming infected with another disease, or make them more vulnerable to having a severe case if they contract an infection. And in this case, it is possible that because of their illnesses, these people were more at risk of becoming infected or becoming ill enough with the infection that they needed medical care.
But Osterholm said it's also possible that if these people had common illnesses, they might have had contact with one another. If that were the case, they still might have all caught the virus from some source, or it might have spread among them.
"The fact that you have so many patients with comorbidities, one has to ask first, what are they? And are you more likely to be sick because of your comorbidities or are you more likely to be in the same place and be exposed because of your comorbidities?"
The first person in this group of cases became ill on April 14. Three days later, two more people got sick. And on April 24, four more people developed symptoms.
The latest three cases were also listed as having "comorbidities." They became ill on April 27, 28 and 30.
Of the 10 cases, nine were men. In fact, so far few women have become infected with this virus -- a detail which may also provide a clue to the route of exposure. Of the 27 confirmed cases, 22 have been men, four have been women and the gender of one case has not been made public. Sixteen of the 27 confirmed cases have been fatal.
Cases have been linked to Saudi Arabia, Jordan, Qatar and the United Arab Emirates. There was a cluster of three cases in Britain, but the first case in the group is believed to have been infected while travelling in Saudi Arabia.
Dr. David Heymann, a professor of infectious diseases epidemiology at the London School of Hygiene and Tropical Medicine, said too little information is known at this point to be able to conclude how these 10 people got infected.
"That number of cases and the fact that they're clustered somehow means that there's either a point source or person-to-person transmission. And that needs to be sorted out," said Heymann, who led the WHO's response to the SARS outbreak in 2003. By point source, Heymann meant that these cases may have been infected from a common source.
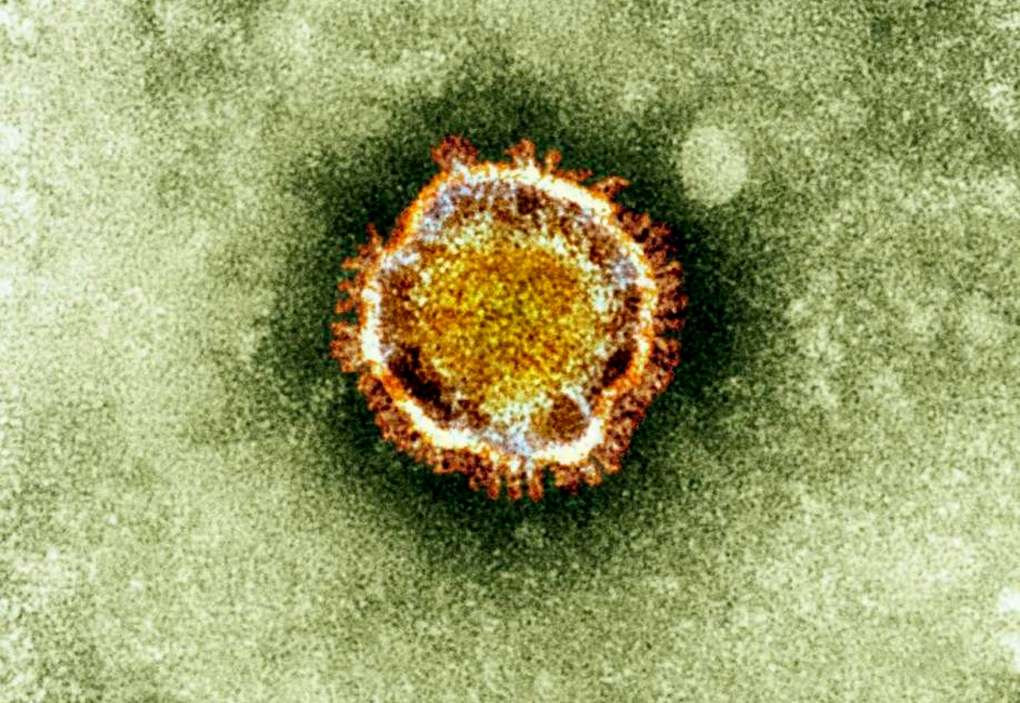
In fact, to this point it remains a mystery exactly how people are becoming infected with this virus, which is a member of the same family as SARS.
"The information that I've seen in the public (domain) does not indicate a source," said Heymann. "And it's very important to know the source."
The closest known relative to the virus is a coronavirus from bats. As these mammals are known to be the source of a number of coronaviruses, it is believed the new virus probably did originate in bats. But how it is jumping from bats to people remains unclear.
There has been some thought other animals may be acting as middle men, as civet cats did in the SARS outbreak. Some coronavirus cases have reported having had contact with animals before becoming ill, with goats and camels mentioned. But many have reportedly had no animal contacts.
Another theory is that bats are perhaps contaminating dates or other palm products. In another disease, Nipah virus, palm wine (sap from palm trees) that is contaminated with bat urine has been identified as the source of some infections.
Marjorie Pollack, deputy editor of ProMED-Mail, said she wasn't surprised to see such a large group of cases, saying she's been wondering for months whether the globe was watching in real time the stuttering steps of a new SARS-like outbreak.
The world was not aware of SARS when it was emerging, but researchers retrospectively pieced together that the virus caused sporadic cases for awhile before it really took off in people.
"I wondered: Will this coronavirus behave in a similar type manner?" Pollack said.
Osterholm said that the world needs to keep an eye on this coronavirus and affected countries need to be transparent about what is going on.
"I think as much as we are focusing with laser-like precision on China and H7N9 (bird flu), this experience just reminds us this could actually be the cause of the next pandemic," he said.
"It may never be possible to stop an emerging coronavirus epidemic from occurring. But I can guarantee you it definitely won't be stopped if there isn't a concerted public health effort with transparency."