The number of children and teens turning up in emergency units with serious mental health disorders is happening in alarming numbers, placing a strain on resources that hospitals say are no longer cutting it.
CTV News surveyed a number of hospitals across Canada and all reported increases in the number of youth seeking help for severe mental illness, such as depression, suicidal risk and behavioural issues.
At McMaster Children’s Hospital in Hamilton, Ont., the local psychiatric emergency room volumes have more than doubled in the last two years, while the inpatient unit has gone from eight funded beds to 22 over the last three and half years.
The IWK Health Centre in Halifax, N.S., reports a 21-per-cent increase in pediatric mental health cases coming to emergency over the previous year.
At the London Health Sciences Centre in London, Ont., the number of urgent pediatric cases have more than doubled over the last decade.
Hospitals are seeing more visits from teens like 14-year-old Courtney, who became severely depressed when bullies taunted her online.
The high-school student would receive anonymous messages with horrible words that tore at her spirit.
“I got a lot of messages telling me that I’m ugly, that I’m fat – that I should kill myself,” she said. “Just a lot of mean things.”
Courtney said she felt embarrassed and alone. “I just felt that nobody else was going through the same thing as me.”
Scared that she would hurt herself, Courtney opened up to her mother and friends. Her family decided to visit emergency at the Children’s Hospital of Eastern Ontario (CHEO), where Courtney was admitted and received daily treatment from a psychologist, psychiatrist and a social worker.
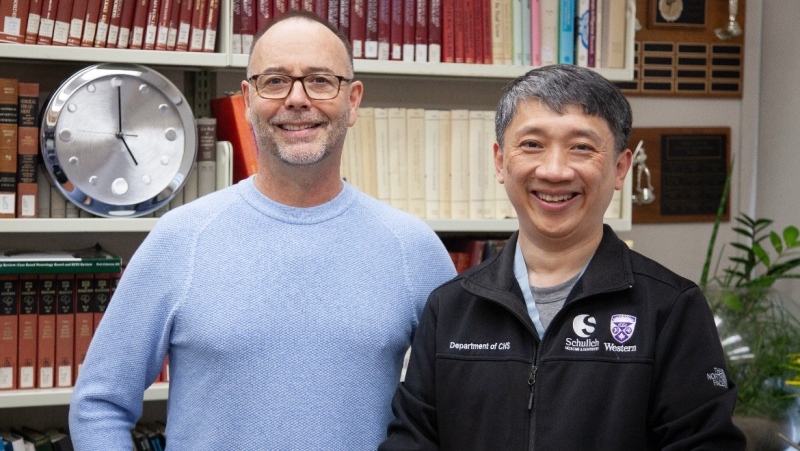
Dr. Clare Gray, head of CHEO’s Crisis Intervention Program, said the emergency room began seeing a surge in young mental health patients a few years ago, with the stats steadily increasing month by month ever since.
Three years ago, the hospital saw 1,600 visits, while this past year, the number was pegged at 2,800.
About half the diagnoses in the emergency units are mood-disorder problems, including depression and suicidal and self-harm behaviours. A smaller subset includes anxiety disorders and substance abuse issues, Gray said.
While she reassured that the numbers indicate more people are seeking help, she’s concerned about how to handle the influx.
“How are we going to manage and assess all these patients and ensure they get to appropriate resources?” she asked.
Dr. Ian Manion, executive director of the Ontario Centre of Excellence for Child and Youth Mental Health in Ottawa, sees the same troubling trends.
“These are not the walking well who are just nervous; these are people with frank illness and are sometimes seeking help for the very first time,” he said.
The demand is taxing mental health services within communities and creating a dramatic rise in wait times for treatment – ranging from six months to a year.
Manion said certain organizations are thinking of closing their year-long wait lists.
Meanwhile, in many communities in Canada, there is a lack of specialized care altogether.
With few or no mental health programs to help families in crisis, they may be referred by default to hospital emergency rooms.
“We have not created systems of care that are organized to meet the demand that’s actually out there in terms of true mental illness,” Manion said.
Gray said the biggest question that medical community has yet to understand is the cause for the upward trend.
But she says part of the answer lies in a de-stigmatization of mental health problems, as related illnesses becomes more mainstream, such as asthma and diabetes.
“I think more people are willing to talk about mental health issues, it’s not a taboo subject,” she said. “Children and parents are obviously communicating their levels of distress.”
However, over a number of years, Dr. Gray has also seen in her own pediatric psychiatry practice a disconnect between parents and children, as people spend more time on their cellphones and computers and less time in each other’s company.
“I think children are really missing that ability to feel valued and feel important in terms of how they’re interacting with their parents,” she said.
The outcome, she said, is children are becoming less resilient, and are losing their ability to handle or manage stressors that come up in their life.
In addition, families are facing multi-generational issues with fewer community supports, says Dr. Sandra Fisman, medical director at London Health Sciences Centre, in London, Ont. Sometimes compounding that is the financial strain in tough economic times.
She said families simply live faster today.
“When I think back to the ease of childhood … life was pretty structured and we always ate at the same time and people seemed to be relaxed and now it is kind of rush, rush, rush,” Fisman said.
The good news is children who are diagnosed and receive treatment quickly have an excellent chance of recovery.
Six months after her treatment, Courtney says she is doing well. She continues with monthly sessions with her therapist, and part of her therapy is artwork.
She said there is no comparison to the place of despair she was in before she sought help.
“I just feel so hopeful about the future and I feel so much happier,” she said. “My advice to anybody who is suffering from depression is to ask for help, because after you just let it all out it’s just so much easier and you feel like a huge weight is lifted off your shoulders.”
But thousands across Canada are still waiting for that help, which is why health care providers must issues a call to action and develop more resources for those suffering from mental illness, Manion said.
“When they start knocking on our door, we better make sure that we have the skills and capacity to meet that need,” Manion said. “Sometimes with young people, you only have one chance.”
A number of communities including CHEO and London Health Sciences are working to meet demand with more community and mobile clinics. Discussions are also underway about putting crisis support online.
Manion says now is the time to take stock of how Canada's health-care system provides such services.
"We don't know how many mental health providers we actually need to meet the demand," said Manion. " Sometimes a crisis pushes us to look at how we ... care for people."
With a report from CTV’s medical specialist Avis Favaro and producer Elizabeth St. Philip