A group of Canadian doctors are on a mission to train their colleagues so that more women can access a minimally invasive type of hysterectomy that has fewer complications than the traditional way of performing the surgery.
Hysterectomies – surgeries involving the removal of the uterus – are the second most-common type of surgery performed on women in North America. Each year, Canadian doctors perform about 50,000 hysterectomies, with 60 to 65 per cent performed as open surgeries.
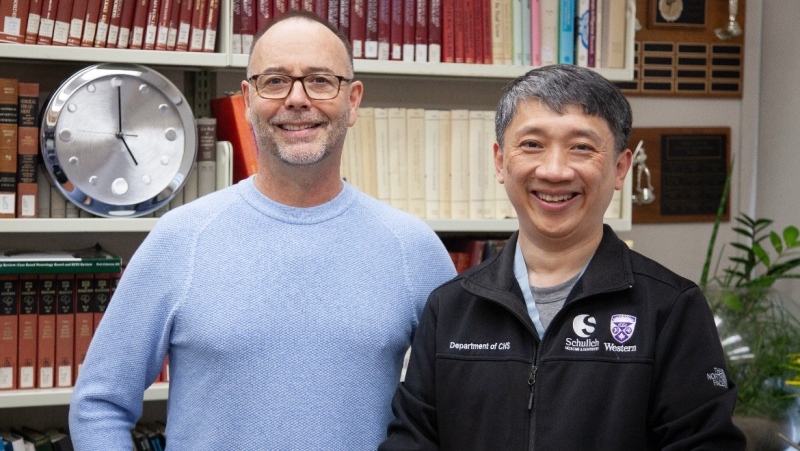
But Dr. Nicholas Leyland, Hamilton Health Sciences' Chief of Obstetrics and Gynecology, said that the major surgery traditionally comes with a host of side effects.
"For open surgery, the disadvantages really are that patients require at least six to eight weeks of recuperation. They have a larger, more unsightly incision, and the incision can create problems and complications," he told CTV News.
But there is a less-invasive way of performing the surgery, known as laparoscopic, or keyhole, surgery. The method involves removing the uterus using just tiny incisions in the abdomen and a camera to guide the doctors through the procedure.
Leyland, who has taught this technique in Canada and around the world, says it is “better for the patient, it’s better for society, it’s better for our economy and it’s certainly better for the health care system,” since patients are in hospital for shorter periods of time.
Dr. Ally Murji, a specialist from Toronto's Mount Sinai Hospital, said women who have laparoscopic hysterectomies recover faster and have fewer complications than those who get the traditional surgery.
"Women who get a minimally invasive hysterectomy return to work quicker, have less pain," he said.
However, the majority of women in Canada do not undergo the newer type of surgery because not enough doctors are trained in the laparoscopic method, Murji noted.
"We need to train gynecologists to do the procedure," he said.
But Leyland said a number of other barriers have prevented health care professionals from providing laparoscopic hysterectomies.
“Hospitals are having a very difficult time now because many hospitals have to cut back on operating room time simply because there isn’t enough money to keep the operating rooms open,” he said.
Laparoscopic surgeries typically take longer than the average surgery, said Leyland.
“So the advantage to doing something faster is clear: if you’ve got a large waiting list of surgeries that have to be done and women are suffering and some surgeons will choose to go the open route”
Despite the barriers, Leyland said “women need to be aware that (laparoscopic surgery) is an option.”
“If the surgeon doesn’t do that procedure, then he can refer that person to a surgeon who does,” he said.
Ontario resident Kerrie Souchotte's doctors recommended she have a hysterectomy after they found fibroids in her uterus. At first, the mother of two said she was worried because she knew the surgery came with serious side effects.
"I knew from hearing stories of other women that it was a long recovery period and had more chance of infections," she said.
But instead, Souchotte opted for a laparoscopic hysterectomy and was able to return home the very next day.
"It was much better," she said. "I was shocked, even in my own recovery. And I think that if I'm the norm, then that would be the preferred way to go."
With a report from CTV News' medical correspondent Avis Favaro and producer Elizabeth St. Philip